Anatomy and Techniques of Skin Grafting
- 1. Anatomy of Skin and Skin-Grafting Dr. Rishi Kumar Gupta M.Ch Resident Department of Plastic and Reconstructive Surgery Gauhati Medical College
- 2. One of the greatest advances in 19th-century surgery was the demonstration that a piece of skin, fully separated from its original site, might survive when transplanted to another part of the body to cover a granulating raw surface.
- 3. • This became possible through the pioneering work of Giuseppe Baronio (1758–1811) from Milan, who performed the first autologous skin graft in a ram in 1804. • Sixty-five years later Jacques Reverdin (1842–1929) carried out the first successful epidermic graft on a human being at Hôpital Necker in Paris, opening a new era in wound-healing management.
- 4. • The route for skin grafting was traced. A few years later, Louis Ollier (1830–1900) transferred a large piece of split-thickness skin, which included the superficial layers and underlying dermis. • Carl Thiersch (1822–1895) and John R Wolfe (1824–1904) made further advances in the procedure. • In the late 1800s, skin grafting became the preferred solution for the management of chronic and granulating wounds.
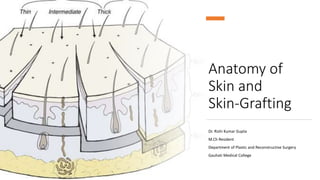
- 5. INTRODUCTION • Skin grafting is a technique for the transfer of cutaneous tissue from one site of the body to another, often to cover large defects. • Depending on the thickness of the dermis of graft that is harvested, skin grafts are defined as full-thickness or split-thickness.
- 6. ANATOMY AND PHYSIOLOGY • The skin represents approximately 8% of our total body weight, with a surface area of 1.2–2.2 m2. • The skin is 0.5–4.0 mm thick and covers the entire external surface of the body. • The main function of skin is to: • Protect body contents from the environment, including pathogens • Maintain temperature • Prevent excessive water loss • Insulation • Sensation, • Immune function • Synthesis of vitamin D
- 7. • Skin loses regenerative capacity when lesioned down to the lower dermis results in scar tissue when injured.
- 8. • Skin has a complex three-dimensional structure characterized by two overlapping layers, the epidermis and the dermis. • The epidermis, as the nervous system, derives after gastrulation from the neuroectoderm. • Epidermis is the outer or upper layer of skin, which is a thin, semitransparent, water-impermeable tissue, consisting primarily of keratinocytes. These cells form a multilayered keratinized epithelium, similar to a wall of bricks.
- 9. SKIN ORIGINS
- 11. ANATOMY OF SKIN
- 13. • The basement membrane separates the epidermis from the dermal tissue and consists of a protein structure produced by basal keratinocytes. • Basal keratinocytes are partially differentiated stem cells of the epidermis that provide the proliferative and regenerative capacity of the skin epithelium. • The epithelium is metabolically active and continuously self-renews to maintain an efficient barrier function.
- 14. • Cellular homeostatic regulation is, as a consequence, very important: too little proliferation would bring a loss of barrier and excessive activity to hyperproliferative disorders, such as psoriasis. • Homeostasis is granted by the basal epidermal cells, which periodically cycle, executing their program of terminal differentiation, a process that takes approximately 28 days.
- 15. • The differentiation of the keratinocytes is characterized by the progressive production of alpha-keratin, with migration towards the surface until the cells lose their intercellular connections (desmosomes), die, and become corneal lamina. • During this process, called “Cornification”, basal keratinocytes produce tonofilaments (precursor of keratin) and then transform into the stratum spinosum as the desmosomes stretch the cells into spikes visible with a microscope.
- 16. • Cells next start to produce Keratohyalin, which aggregates in dense and basophilic granules, giving the name to the stratum granulosum. • In these granules a histidine-rich protein, profilaggrin, becomes progressively filaggrin, which ultimately acts as a glue to keep keratin filaments together once the cells die and the cell membrane degrades. • As the cells divide and move up through the epidermis eventually transform into the stratum corneum a layer of dead cells, which ultimately is highly mechanically and chemically resistant due to chemical bonds between lipids and proteins.
- 17. • Also contained within the epidermis are melanocytes, Langerhans cells, Merkel cells, and sensitive nerves. • Melanocytes: • 10% of the epidermal • Derived from the neural crest. • Produce melanin granules (contained in the melanosomes) • Providing color to the skin and protecting basal epithelial nuclei from ultraviolet damage. • They are anchored to the basal lamina by hemidesmosomes, but do not have desmosomic connections with other cells.
- 19. • Langerhans cells: • Situated in the Stratum spinosum • Immune cells Antigen presenting cells. • Playing an important role in allograft rejection and contact dermatitis. • Merkel cells: • Reside in the Basal layer • Are commonly found in the epidermis of palms, soles, nail beds, oral and genital areas. • They act as mechanoreceptors and thus are responsible for neurosensory transmission.
- 21. • Skin adnexal structures: • Epidermal derivatives that invaginate into the dermis with a lining of epithelial cells. • Eg: Hair follicles, sweat and sebaceous glands. • These structures provide the basis for re-epithelialization following the harvest of an STSG. • Sensitive nerve supply to the skin is rich and extends through the basement membrane into the epidermis. • Nerve fibers also go to skin adnexal organs that allow hair to become erect and sweat glands to secrete.
- 22. DERMIS • The dermis is a tough fibrous layer that provides the mechanical features of the skin. • It is composed primarily of collagens, glycosaminoglycans, and elastins. • Skin grafts without the dermis result often unstable skin. • Grafting a part of the dermis is therefore very important to consider in terms of functionality of the future skin.
- 23. • Papillary dermis: • Upper part of the dermis • Contains blood vessels and nerve fibres. • Consists of fine collagenous fibres that form an undulating interface with the overlying basement membrane and epidermis. • This increases the contact area between dermis and epidermis • For maximal mechanical stability of the two layers • Exchange surface for diffusion.
- 24. • Reticular Dermis: • Deeper • Increasingly thicker collagenous fibers (mainly of type I) as we move toward the subcutaneous tissue. • It has larger collagenous fibers with substantial strength. • The mechanical properties of the dermis are • Critical to allow movement while providing stability and protection from mechanical trauma. • The dermis is remarkably self-healing, mainly due to the presence and activation of myofibroblasts following injury.
- 25. BLOOD SUPPLY TO THE SKIN • Dermal vascularisation is particularly important, as blood vessels are not directly present in the relatively more metabolically active epidermal layer, glands, and hair follicles. • Blood vessels set up a rich superficial plexus just underneath the basement membrane in the papillary dermis, facilitating nutrient transport to the epidermis. • The blood vessels in the papillary dermis are arranged in the papillary plexus, with a rich network of capillaries in the papillae, which come in close contact with the epidermis.
- 26. • Deeper in the dermis is the reticular plexus from which small vessels distribute to the subcutaneous and deep dermal tissues to vascularize adnexal organs, including the hair follicle bulb. • Blind-ended lymphatic structures are present in the dermis from where they connect to the reticular plexus and to larger vessels in the subcutaneous tissue.
- 27. • In this Subcutaneous region, lymphatic vessels are larger, with valves, and drain in deeper lymphatic vessels called regional collectors. • In the skin the lymphatic drainage is very active with multiple interconnections enabling lymphatic exchange. • Circular skin and subcutaneous damage can therefore lead to problematic lymphatic stasis in extremities or in the genital area.
- 28. STEM CELLS AND REGENERATION OF SKIN • Basal epithelial keratinocytes are the committed stem cells of the epidermis. Constant self-renewal provides a new protective layer at the skin surface. • Hair follicles contain multipotent stem cells that are activated upon the start of a new hair cycle and upon wounding to provide cells for hair follicle and epidermal regeneration. • In the hair follicle stem cells reside in the bulge area. Bulge cells are relatively quiescent compared with other cells within the follicle.
- 29. • However, during the hair cycle, bulge cells are stimulated to exit the stem cell niche, proliferate, and differentiate to form the various cell types of the hair follicle. • Clinical Significance: • Bulge cells can be recruited during wound healing to support re-epithelialization.
- 30. GLANDULAR STRUCTURES • Sebaceous glands are small saccular structures residing throughout the dermis but are more common in thicker areas. • These glands produce lipid-rich sebum on the surface of the skin and around the hair shaft. • Sebaceous glands are particularly large on the face, trunk, shoulders, and genital and perianal regions.
- 31. • Sweat glands are divided into eccrine and apocrine glands. • There are numerous eccrine glands in every region of the body except the tympanic membranes, lips, nail bed, nipples and clitoris.
- 32. SCIENCE
- 33. MECHANISMS OF SKIN GRAFT TAKE • Skin grafting is the transfer of autologous skin cells left in anatomic order but without an intact blood supply. • Therefore, time and the recipient surrounding conditions limit the vitality. The operative procedure allows for nearly immediate coverage of large wound areas. • Meshed grafts allow further expansion of skin but leave multiple small wounds that are re-epithelialized, mainly from the mesh within a few days. • Skin can also be expanded through multiple small skin island grafts (as in Reverdin’s technique) that stimulate granulation tissue, probably by excreting growth factors. • In STSGs, keratinocytes on the basal layer show high proliferation rates, which may ultimately stimulate growth factor excretion.
- 34. • Three phases of skin graft take are commonly described: 1. Serum imbibition; 2. Revascularization; 3. Maturation
- 35. SERUM IMBIBITION • In the first days, before the graft revascularizes, oxygen and nutrients diffusing through the plasma between the graft and the wound bed will nourish the skin graft. • Huebscher in 1888 and Goldmann in 1894 theorized that skin grafts might be nourished by host fluid before vascularization of the graft occurs. They referred to this as “plasmatic circulation.”
- 36. • Later, Converse et al. altered the term to “serum imbibition,” as fibrinogen changes into fibrin that fixes the skin graft on to the wound bed in the absence of real plasmatic flow. • Converse’s studies show that skin grafts gain up to 40% of their initial weight within the first 24 hours after grafting and then this gain is reduced to 5% at 1-week post grafting. • In the first hours, passive absorption of serum from the wound bed causes oedema, which resolves when the revascularization is functional.
- 37. REVASCULARIZATION • Revascularization is critical for long-term skin graft survival. • Early studies in the 19th century suggested a connection between the wound bed and graft vessels, referred to as inosculation, but the mechanism of revascularization remained unclear for many years. • Three hypotheses of revascularization are supported by the literature, each of them probably contributing to the process: 1. Anastomosis, 2. Neovascularization 3. Endothelial cell ingrowth
- 38. • Anastomosis: The process of reconnection between the blood vessels in the recipient site wound bed and the graft. • Neovascularization: It is characterized by new vessel ingrowth from the recipient site into the skin graft. • Endothelial cell ingrowth: It describes endothelial cell proliferation sliding from the recipient site, utilizing pre-existing vascular basal lamina as a structure, while in the graft endothelial cells gradually degenerate.
- 39. • The process of revascularization begins as early as 24–48 hours after grafting. • There is vessel ingrowth mainly from the wound bed and less so from the wound margins, since no significant increase in blood vessels was seen in graft margins after skin grafting. • Studies by intravenous injection with radioisotopes that blood flow in the graft was established 4 days after grafting. • Similarly, studies using India ink showed graft vessel stain as early as 2 days postgrafting.
- 41. MATURATION • Once the skin graft is completely integrated, the same graft and surrounding tissues remodel and contract, similar to the last phase of wound healing after re-epithelialization is complete. • Skin grafts take at least 1 year to complete maturation, with the extension of this process continuing for several years in burn victims and children. • Scars from skin grafts can continue to improve for a number of years, often making prolonged conservative therapy worth considering.
- 42. • Skin graft vascularization contributes to prevent underlying tissue contraction. • Fibroblasts from surrounding tissues and from blood circulation become activated and repopulate the wound at the interface between the graft and the recipient site. • As collagen is deposited, cross-linking allows the extracellular matrix to resist mechanical insults.
- 43. • During wound maturation, the epithelium from the edges of the wound produces a basal lamina on the open surface while sliding across progressively covering the immature granulation tissue. • During the re-modeling phase, all immature blood vessels necessary to support the initial phases regress and eventually disappear. • The re-modeling phase of wound healing is the longest, lasting from several months up to years.
- 44. SKIN APPENDAGES AND FUNCTIONAL STRUCTURES • Hair follicles, sweat glands, and dermal nerves can often be transferred within thick-STSGs and full thickness skin grafts. • Thin STSGs will not allow the transfer of hair or other adnexal glands, as the regenerating bulb is not harvested. • Hair regrowth can occur in STSGs but, due to the shallow depth of harvest, is rather unlikely. Full-thickness and composite grafts will show hair regrowth 2–3 months after grafting.
- 45. • It is still unclear how nerves regrow into the skin graft. Studies demonstrated that recipient nerves use the basal lamina infrastructure of degenerated blood vessels and Schwann cells of donor nerves to grow. • Although histological images reveal similar neural structures between healthy skin and integrated skin grafts, patients report abnormal sensation, including hypersensitivity and pain, up to 1 year. • Usually, patients regain sensitivity of the grafted area after 1 year, but the result is not completely normal.
- 46. • Neural reconnection to sweat glands will reactivate their function up to 3 months after grafting. • For this reason, moisturizing of the skin graft is advised for at least 3 months to avoid dryness. • Full-thickness skin grafts include skin appendages that can survive and be functional at the recipient side, while STSGs do not contain the deep structure skin appendages and remain without glandular function or hair growth.
- 47. CLINICAL APPLICATION • Skin wounds that extend into the deep dermis heal through the mechanisms of scarring and wound contraction. • Also, wounds that are left open for months to years can degenerate into skin cancer (Marjolin’s ulcer). • For these reasons, methods that rapidly facilitate wound coverage or resurfacing are desired.
- 48. • Skin grafting is still the gold standard to cover large areas of skin loss. • The concept is to take skin from an area where the donor site will heal with minimal scarring and transplant it to an area of need. • As skin grafting always leaves some sort of scar, donor site considerations are important when balancing the needs of the recipient site for a given skin graft.
- 49. • Skin grafts can be: • Of different origin from different anatomical sites • Can be harvested in different thicknesses • Depending on the histological level of the graft the skin graft type is classified by: • Thin and thick STSGs, • Full-thickness skin grafts • Composite grafts
- 50. Thickness in mm Name Thin 0.15–0.3 Thiersch–Ollier Intermediate 0.3–0.45 Blair–Brown Thick 0.45–0.6 Padgett Full Thickness >0.6 Wolfe–Kraus Skin grafts are further classified according to their thickness into:
- 55. • The thickness of the dermal layer classifies the STSG as either thin or thick. • An STSG consists of epidermis and a variable amount of superficial to profound (papillary) dermis. • As the dermis is responsible for the viscoelastic property of the skin, it is crucial for stability of the future skin. • The amount of dermis grafted is key to the outcome: body areas with high mechanical friction are ideally grafted with thicker dermal layers.
- 56. • Thin STSGs include the epidermis and a thin layer of the dermis. • STSGs are commonly taken from the lateral thighs and trunk. • They do not include the full length of appendages and are therefore unlikely to grow hair or to develop full sweat gland function. • Advantage of thin STSGs: • Reduced morbidity of the donor site • Possibility of performing multiple harvests from the same donor area about 2 weeks after the previous harvest. • Although thinner grafts allow for more frequent re-harvest, they result in additional wound contraction.
- 58. • Thick STSGs include more dermis with a greater number of full hair follicles and glandular structures. • These grafts will likely develop some hair growth and sweat gland function about 2–3 months after grafting. • Thick STSGs are commonly selected to cover areas of high mechanical friction, such as joints, plantar soles, and the palm. • Since hair regrowth is common in thick STSGs, the donor site should be carefully chosen to avoid unpleasant hair growth.
- 59. • Because of decreased nutrient diffusion, thick grafts require a better recipient wound than thin grafts during the revascularization process. • Therefore, thick grafts should be avoided in unhealthy wound beds such as in chronic ulcers. • The donor site usually heals with more obvious scarring and discoloration but less graft contraction.
- 61. • To increase the uniformity and expedite the harvest of skin grafts, a number of electrical or air-powered dermatomes have been designed to take uniform small to large skin grafts. • Powered dermatomes have adjustable guards to set the graft thickness. • Drum dermatomes are precision instruments that can take large graft areas reliably. • They require placement of adhesive on the skin and an oscillatory movement by the operator.
- 62. • When possible, harvesting the skin graft first and covering the donor site will avoid contamination from the wound. • The size of the graft needed should be accurately measured prior to harvest. The graft thickness can be adjusted by a lever near the end of the dermatome between 0.1 and 1.0 mm. • The surgeon presses the dermatome in 45°to the skin surface on to the tissue and moves the device from distal to proximal with uniform pressure and speed.
- 63. • Keeping the graft moist with saline-impregnated gauze is of vital importance if not immediately grafted. • Larger skin grafts should be incised with an 11 knife multiple times to allow wound fluid drainage and prevent collections between the skin graft and the wound bed.
- 64. MESHED SKIN GRAFT • STSGs can be enlarged up to six times their original size. • Enlargement of the graft can vary from just a few manually applied perforations with an 11 blade to a systematic enlargement with a hand- powered meshing device (Mesher) that applies multiple slits at regular intervals • Meshed grafts are often used following large burns when the wound area exceeds available healthy donor sites.
- 65. • Meshed skin grafts are also very helpful to cover irregular geometric surfaces such as around joints as they minimize folds in the graft. • Development of contractures should be taken into consideration in functional areas. • Using different mesh templates, from 1 : 1 to 1 : 9, can regulate the extent of the enlargement of meshed grafts. • The most commonly used mesh ratio is 1 : 1.5 in smaller wounds, while a mesh ratio of 1 : 3 and 1 : 6 is often needed to cover large burns.
- 67. • The mesh gaps will be subsequently filled by keratinocytes from the skin stripes. • This process takes longer with higher mesh expansion ratios. • Since grafted cells excrete growth factors, underlying granulation tissue will be stimulated until full re- epithelialization occurs. • Aesthetically unpleasant hypergranulation in the open areas of the mesh are therefore more often seen in large mesh ratios.
- 68. • Meshed skin grafts leave unsightly long-term results that need to be considered when selecting this technique. • Very thin meshed skin grafts used in combination with dermal substitutes or keratinocyte cultures are other strategies to mitigate the result.
- 69. FULL-THICKNESS SKIN GRAFT • Full-thickness skin and composite grafts are limited in availability but show excellent function and sensitivity after engraftment. • Full-thickness grafts should be considered in the reconstruction of aesthetically dominant (face) or functionally important areas (hand). • • Full-thickness grafts from the retro-auricular region and above the eyebrows are an excellent choice to maintain tissue quality and colour of the surrounding skin in the face.
- 71. • If needed, foreskin can also be used and in adults' retro-auricular skin is helpful in face reconstruction. • Also, excess skin from the upper eyelid and submental area can be taken into consideration for full-thickness reconstruction if the patient is comfortable with an aesthetic-like intervention. • In hand reconstruction, elbow crease and wrist fold grafts have been described but should be avoided in cultures where these donor site scars may result in stigmatization of the patient as they can be associated with suicide.
- 72. • Hypothenar skin is useful for glabrous reconstruction but can leave a painful scar that can cause an unpleasant sensation if the hand is positioned on a table in a relaxed position. • Therefore, full-thickness skin graft from the hypothenar area should be harvested elliptical with the main axis and slightly more dorsal in relation to the glabrous–skin border.
- 73. • Full-thickness skin grafts are taken in an area where loose surrounding skin is available to achieve primary closure. • Skin grafts can be designed elliptical and excised with a knife. • Harvesting should be carried out trying not to elevate the underlying tissue. • Most of the fullthickness grafts need defatting and this can be easily performed by spreading the graft over the index finger and trimming the fat tissue tangentially to the skin. • Defatting of the graft will encourage graft take.
- 75. COMPOSITE GRAFT • Composite grafts include a layer of subcutaneous fat tissue under the dermal and epidermal layer. • The donor sites are principally the same as the full-thickness donor sites. • Since fat tissue is less vascularized and more vulnerable to ischemia, optimal revascularization is needed in order to achieve graft survival. • Composite grafts can be used in children as they show a remarkable capacity to revascularize thicker grafts. • Some surgeons use composite grafts to reconstruct the nasal tip, the alar, and the columella in cleft lip patients.
- 76. SKIN FIXATION AND DRESSING • Once the autologous skin is grafted on to the wound site the revascularization depends on multiple factors. • One of the most important factors to achieve stable taking is the immobility of the graft during the revascularization process. • An “Open-technique” requires labor-intensive monitoring on the graft and any fluid that is formed beneath the graft is rolled out with a cotton-tipped applicator. • More often, skin grafts are fixed through a series of sutures and overlying compressive dressing materials (Bolster).
- 78. • Vacuum-assisted pressure devices can be used with a protective interface of petroleum gauze or a silicone sheet to permit continuous compression on to the graft and fluid removal. • The suction dressing is especially useful if fast mobilization is desired in patients with wounds in joint regions or the lower extremities. • Compression to stabilize the graft on to the wound bed should be performed until 5–10 days when the graft is usually stable and wound areas are completely closed.
- 79. • Splints can be used as adjuncts if the risk of wound contraction is high, such as in chin scar release or in joint and web space release of the hand. • These splints or casts should be worn up to several months after grafting, in the beginning 24 hours per day, later during the night, to avoid the loss of mobility. • Physiotherapy and scar massage are also important elements for obtaining better results with skin grafts.
- 80. SEALANTS • Fibrin glue can also be helpful to assist skin graft fixation. • In this case, some surgeons spray fibrin glue on to the skin graft dermis just before placing it on to the wound site. The fibrin network may even act as a provisory extracellular matrix under the graft.
- 81. FIRST DRESSING CHANGE • The first dressing change should occur once the skin graft is revascularized and has a stable physical connection to the wound bed. • • Early dressing change around the third day after grafting may allow predicting the “take rate” of the graft but risks secondary graft loss through shear forces that disturb nascent vessel connections. • More commonly the dressings are taken off for the first time 5–10 days after grafting.
- 82. RECIPIENT SITE CONSIDERATIONS • Before planning a skin graft, several factors have to be taken into consideration to achieve optimal tissue cover at the wound site. • The wound bed quality has to be optimized for a successful “take” of the graft and the skin color, thickness, and mechanical resistance of the donor site area should ideally match the recipient site skin quality. • Wound conditions often found in chronic or insufficiently debrided burn wounds and characterized by low wound bed vascularization or high bacterial loads will not allow skin grafts to be taken.
- 83. WOUND BED PREPARATION • A good quantity of blood vessels near the surface is critical in order to support graft viability. • If highly vascularized peritendon and periosteum are still intact, skin grafts can be performed. • In chronic wounds: • Re-epithelialization occurs at the wound margins that can grow into the tissue and may inhibit the lateral reconnections of the graft. • Therefore, wound margins should be sharply excised with a blade before grafting.
- 84. • Experimental data suggest that the bacterial level must be brought down below the critical level of 105 bacteria per gram of tissue to allow a skin graft to take. • Surgeons have learned over time that a “Granulating” wound has a high likelihood of taking a skin graft. • Active bleeding of the wound bed will likely lead to blood collection between the graft and the wound bed, inhibiting graft take. • Accurate homeostasis can be performed with bipolar cautery and larger blood vessels can be ligated with fine resorbable sutures.
- 85. • Small areas of tendons and bones can either be prepared by vacuum- assisted closure therapy to grow granulation tissue from the sides or dermal substitutes can be used to cover functional structures.
- 86. FUNCTIONAL CONSIDERATION • Consideration needs to be given to the size of graft needed, the degree of wound contraction expected, the color and texture of the skin required, and the need for adnexal glands. • The amount of wound contraction expected is inversely related to the amount of dermis in the skin graft. • Full-thickness skin grafts are frequently used for nipple–areola reconstruction, syndactyly release, or ectropion release. • Full-thickness grafts are in short supply and can be augmented by tissue expansion prior to harvesting full-thickness skin grafts.
- 87. • Very thin grafts such as epidermal grafts result in a donor site that heals quickly with minimal contraction but provide little constraint to wound contraction. • The surgeon can use this as an advantage if wound contraction is desired. For example, on large scalp wounds or abdominal wounds, wound contraction may be desired to keep the skin graft as small as possible while pulling the wound edges together over time.
- 88. AESTHETIC CONSIDERATIONS • Skin color is determined by a complicated integration of skin texture, melanin pigmentation, and blood flow. • In general, replacement of tissue from a similar or adjacent site will give the best color match. • In the face, this is often the most critical aesthetic area and choosing donor sites such as supraclavicular, posterior auricular, upper eyelid or scalp skin grafts can often lead to an excellent color match.
- 89. • Skin texture is most commonly an issue when dealing with glabrous skin (palms and soles of feet). • In this case, placing a non-glabrous skin graft to cover these areas can result in a very unnatural look • Glabrous skin grafts are obviously in short supply but can be harvested from the hypothenar eminence.
- 90. DONOR SITE CONSIDERATIONS • The obligatory scarring or discoloration associated with donor sites must be considered when taking a skin graft. • Common donor sites include the thigh, trunk, and buttocks, regions frequently covered by clothing. • Full-thickness donor sites in the head and neck are pre- and postauricular regions (the first is generally thicker), nasolabial crease, supraclavicular region, eyelids, and neck. • Other common regions include the inguinal crease that is often used to cover large defects. In this case it is important to harvest laterally and away from potentially hair-bearing regions of the pubis. This area generally heals well and is hidden.
- 91. DONOR SITE DRESSING • Topical gauze soaked with diluted epinephrine solution is useful to stop bleeding at the donor site and can be left until the operation is ended, adding an analgesic effect. • The donor site of an STSG generally heals (re-epithelializes) in 7–21 days depending on the size and depth of the graft taken and the age of the patient. • A myriad of donor site dressings are available with multiple studies on a variety of products.
- 92. • Traditionally, fine-meshed gauze, often impregnated with a petroleum- based product, is placed over the wound and fixed in place. • Cotton gauze is placed over this and removed a day or two after the operation. • The wound heals under this dressing and the dressing spontaneously comes off when healed. • The advantages of this type of dressing system are its simplicity, low cost, and minimal wound care requirement.
- 93. • A large number of other dressings, including silver based, absorptive, and biological, have been studied. • In most of the cases the donor site heals spontaneously, thus simple impregnated gauze is still the gold standard.
- 94. SKIN GRAFT STORAGE • Skin grafts can be stored on a moist gauze at 4°C for up to 2 weeks, although the viability decreases over time. • Experimentally, storage can be extended using cell culture media. • For degloving injuries, the skin can be defatted acutely and reapplied as a full-thickness graft.
- 95. COMPLICATIONS 1. Hematoma 2. Seroma 3. Infection 4. Non-take 5. Wound Contraction 6. Instability 7. Cosmetic issues 8. Doner Site
- 96. HEMATOMA • Any liquid between the wound and skin graft can impair skin graft take. • Since bleeding represents one of the most important complications after excision and grafting with up to 100–200 mL of blood, every 1% of body surface area that is excised, particularly from the scalp.
- 97. • The surgeon must be certain that bleeding has stopped prior to dressing the wound. Suture ligation or cautery can be used to control larger bleeding vessels; oozing can be controlled with pressure and/or pharmacological methods such as topical thrombin, epinephrine, or fibrin glue. • To reduce bleeding during excision the area can be primarily injected with epinephrine diluted in saline (tumescent technique). • As discussed above, incisions of the graft should be done to allow fluid evacuation through a compressive or suction dressing.
- 98. SEROMA • Serum imbibition is essential for early skin graft survival. • Excessive serum, such as a seroma, will prevent or delay skin graft take. • Seromas are better tolerated than hematomas, and adequate fenestrations (pie crusting) can prevent this problem.
- 99. INFECTION • When skin graft infections occur, pus often accumulates beneath the skin graft and can rapidly spread. • If an infection is found early, prompt incision and drainage of the fluid beneath the graft can often salvage some or all of the skin graft. • A large number of dressings have been developed that carry a variety of topical antimicrobial agents. • Silver nitrate, mafenide acetate, and silver ion dressings are commonly used. • Bacteria seem not to develop resistance easily to silver products, making these products desirable.
- 100. NONTAKE • Unfavorable conditions: 1. Malnutrition, 2. Vasculitis 3. Malignant diseases 4. Steroids 5. Chemotherapeutic medications
- 101. WOUND CONTRACTION • Wounds covered with skin grafts can still undergo wound contraction leading to a scar contracture. • After the acute inflammation phase the contraction starts. • Fibroblasts from surrounding tissues and from blood circulation start to be activated repopulate the wound between the graft and the wound bed. • Collagen deposition allows wound maturation. • Collagen is deposited cross-linking occurs extracellular matrix becomes mechanically resistant.
- 102. • This increase in mechanical resistance allows mechanical interaction with fibroblasts that develop fibers called alpha-SMA. • The development of alpha-SMA coincides with • Fibroblast Myofibroblast
- 103. INSTABILITY • Shear forces are a major cause of skin graft failure that can disrupt the nascent fragile blood vessel connections. • Later, thin skin grafts have less collagen content and are prone to delamination due to shear forces.
- 104. COSMETIC ISSUES • Unpleasant net-like patterns of meshed STSGs are much more prominent than non-meshed or full-thickness grafts. • Color differences are a common problem if donor sites could not be optimally chosen.
- 105. DONOR SITE • Infection at donor sites can occur from bacterial contamination during the operation or in the postoperative period. • These infections are treated with topical antimicrobial agents, including silver dressings. • The delay in healing of donor sites due to infection can lead to hypertrophic scar formation. • Hypertrophic scar or keloid formation can also result from deep donor sites or in patients with a propensity for scarring. • Itching is a common reaction to donor sites as well as hypersensitivity to changes in temperature.
- 106. FUTURE
- 107. DERMAL SUBSTITUTES • Burke et al. first described a collagen–glycosaminoglycan scaffold to treat dermal defects in the early 1980s. • Dermal substitutes are widely used in large burn injuries, when skin lesions are so extensive and unaffected donor skin areas are often limited. • Cadaver skin (allograft) or dermal substitutes can be used initially to cover large defects.
- 109. • Dermal regeneration is very limited in our skin and full-thickness skin defects heal by secondary intention with scar tissue formation. • The difference of scar tissue and healthy skin besides the aesthetic appearance is the viscoelasticity and therefore stability • Scar tissue shows histological parallel-oriented collagen fibers, while healthy dermis consists of randomly oriented collagen fibers.
- 110. • In some patients and for restricted donor sites keratinocyte cultures or very thin STSGs can be attempted to close full-thickness defects. • Integra: • The first commercially available skin substitute • Bovine-derived collagen type 1 cross-linked matrix with glycosaminoglycans • Similar to the dermal structure and covered by a silicone sheet to recreate temporarily the function of the epidermis. • Can be applied to a vascularized wound bed blood vessels and cell growth into the collagen matrix create a vascularized neodermis after 2–3 weeks.
- 111. • During the avascular period, the dermal graft is very sensitive to infection, one of the main disadvantages of the two-step strategy. • Once revascularization is accomplished, the silicone layer can be removed, and the epidermal replacement can be granted by either keratinocyte cultures or a thin STSG. • Newer clinical studies show that small areas of exposed tendon or bone without remaining peritendineum or periosteum can be successfully grafted with Integra.
- 112. • Matriderm: • (Dr. Suwelack Skin and Health Care), a bovine-derived collagen matrix with noncross-linked collagen fibers of types I, III, and V matrix coated with elastin fibers. • Allografts and xenografts will be rejected by the recipient and may adhere in patients with large burn injuries for several weeks because of the posttraumatic immunosuppressed stage.
- 113. • After 2–3 weeks dermal dressings will be removed and a well- vascularized wound bed is found underneath that is ready for final skin reconstruction by autologous grafts. • Another drawback for human- and porcine-derived dermis is possible viral infection transmission.
- 114. CELL CULTURES • Epithelial cell culture autografts were first introduced by Rheinwald and Green in 1975 and pose a milestone in skin regeneration. • In patients with extensive burns, donor sites are often limited. • Cultured epithelial autografts (CEA) are keratinocytes harvested from a small biopsy of the same patient that are then expanded manifold in the laboratory.
- 115. • The time needed to expand keratinocyte cultures in vitro for clinical use is dependent upon the delivery method. • In order to obtain sheets of confluent keratinocytes as in normal epidermis, it may take up to 5 weeks. • This time can be shortened to less than 2 weeks by expanding the cultures on bio-scaffolds that allow cell attachment and proliferation prior transplantation. • Hyaluronan or collagen scaffolds • Cell suspensions : the in vitro time to only 5–7 days.
- 116. • The introduction of CEA in clinical practice dates back more than 20 years, but the best delivery method as well as efficacy and indications has not been identified yet. • Published studies have reported taking rates of CEA on biomaterials varying from 0 to 80%, raising many questions about their effectiveness.
- 117. BIOENGINEERED CULTURED ALLOGENIC BILAYERED CONSTRUCTS • Cell-seeded skin constructs were first described in the early 1980s, when autologous keratinocytes and fibroblasts were seeded into collagen glycosaminoglycan matrixes by centrifugation. • Further research found neonatal skin cells to be very efficient in accelerating wound healing. • Neonatal foreskin keratinocytes and fibroblasts were than used in combination with biological or synthetically engineered scaffolds to stimulate wound healing in topically applied allogenic skin constructs.
- 118. • Apligraf: • (Organogenesis, Canton, MA, US and Novartis Pharmaceuticals, East Hanover, NJ, US) is a • Bilayered living skin-equivalent composed of type I bovine collagen and allogenic keratinocytes and fibroblasts obtained from neonatal foreskin.
- 119. • Fibroblasts are cultured in the collagen matrix where they proliferate and augment the extracellular matrix with all kinds of proteins. • Keratinocytes are then added and build up the epidermal layer. The living skin construct supports skin graft take in difficult wounds, such as burn wounds, or accelerates healing in chronic wounds. • With a shelf-life of 5 days at room temperature Apligraf has to be applied fresh either as a temporary dressing or over meshed STSGs.
- 120. • Dermagraft: • (Advanced Tissue Sciences, La Jolla, CA, US) does not contain keratinocytes and is described as a living dermal skin construct consistent with a cryopreserved bioabsorbable polyglactin mesh seeded with allogenic neonatal fibroblasts.
- 121. THANK YOU
Editor's Notes
- Synthetically dermal substitutes such as Integra and Matriderm are permanent dermal regenerative templates that will be ultimately covered by an epidermal autologous graft.