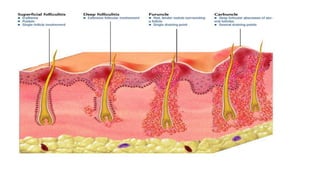
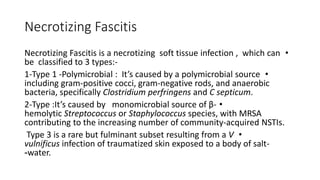
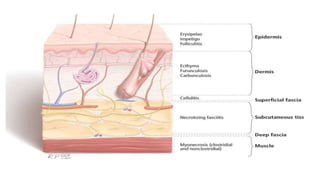
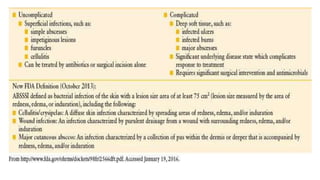
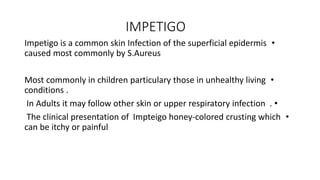
Soft tissue infections can range from mild to life-threatening. Common causes include Staphylococcus aureus and streptococci. Management depends on the type and severity of infection. For minor infections like impetigo or folliculitis, topical or oral antibiotics may suffice. More serious infections like cellulitis may require hospitalization and intravenous antibiotics. Necrotizing fasciitis is a grave infection involving tissue death that requires aggressive surgical debridement and broad-spectrum antibiotics to prevent high mortality rates.
![Management of Impetigo
•
Topical therapy (e.g : Mupirocin) for impetigo should be administered if there are
a limited number of lesions.
•
Extensive impetigo: requires treatment with systemic antibiotics . Unless
cultures reveal only beta-hemolytic streptococci (usually group
A Streptococcus [GAS]), the oral antibiotic prescribed for impetigo should be
effective for the treatment of both S. aureus and streptococcal infections(e.g :
Cephalexin and dicloxacillin)
•](https://image.slidesharecdn.com/softtissue-240313161721-d27dc857/85/SOFT-TISSUE-abscess-and-other-8-320.jpg)