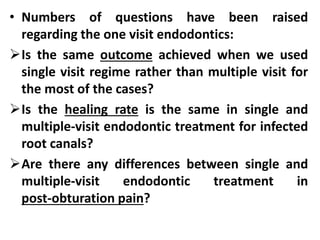
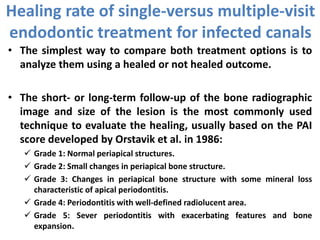
This document discusses single-visit versus multiple-visit endodontic treatment. It notes that advances in technology have increased the feasibility of single-visit treatment by making procedures more effective and efficient. However, questions remain about outcomes and healing rates between the one and multiple visit approaches. The key factors in bacterial elimination and healing are thoroughly debriding the canal and removing or inactivating bacteria and their byproducts like endotoxins. Calcium hydroxide dressing between visits may further reduce bacteria and neutralize endotoxins. Overall, outcomes may depend on a case's complexity and ability to sufficiently disinfect the canal, with multiple visits potentially enabling better cleaning for difficult cases.