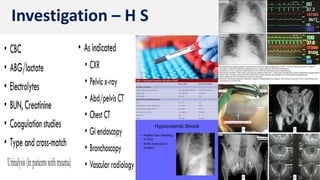
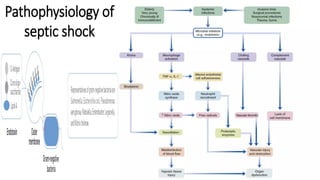
The document outlines the definitions, classifications, causes, and treatment options for hypovolemic and septic shock, highlighting the significance of timely intervention to prevent cell death caused by inadequate oxygen delivery. It emphasizes that septic shock, a severe condition arising from infections, primarily affects vulnerable populations such as children and the elderly, with a mortality rate of 25-50%. Additionally, it presents various clinical scenarios and questions to reinforce understanding of shock types and management strategies.
![Prof. U. Murali.
Shock
[Hypovolemic | Septic]](https://image.slidesharecdn.com/shock-septichypovolemic-240117054434-ebc327f8/85/Shock-Septic-Hypovolemic-Causes-Management-1-320.jpg)


































![A patient presents with hypotension and clinical features of septic shock.
Despite insertion of a CVP line the resident doctor is unclear whether the
patient’s hypotension is caused by hypovolemia (or) by sepsis-induced
myocardial depression [MD]. Which of the following statements is true? –
◼ a) An IV fluid must not be given unless MD is absolutely excluded.
◼ b) The resident should rapidly administer 500 ml of fluid to differentiate
between hypovolemia & MD.
◼ c) The resident should first raise the pressor support & see if the patient
responds.
◼ d) MD is not a component of septic shock, and the resident should only
treat for hypovolemia.](https://image.slidesharecdn.com/shock-septichypovolemic-240117054434-ebc327f8/85/Shock-Septic-Hypovolemic-Causes-Management-38-320.jpg)








