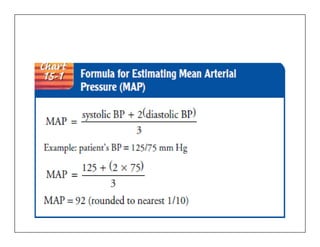
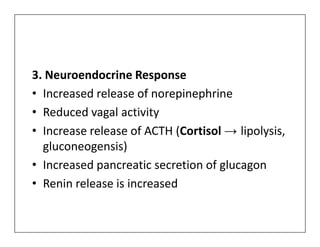
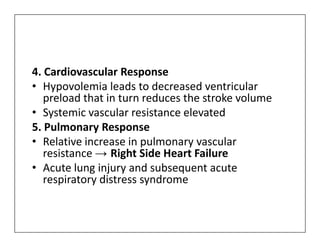
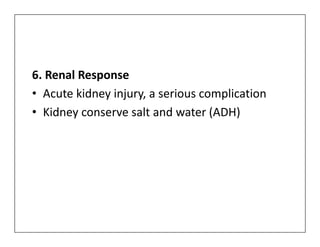
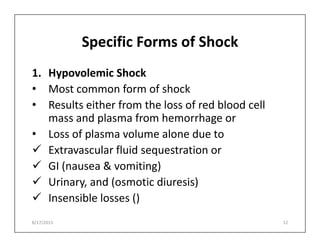
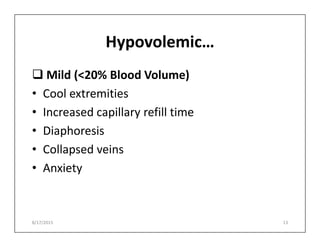
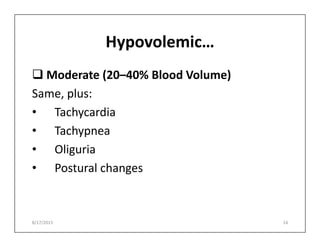
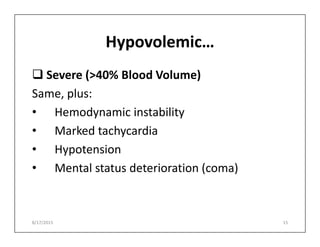
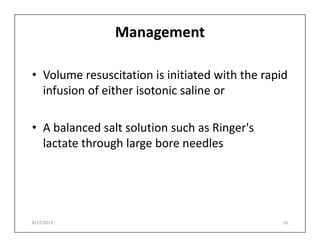
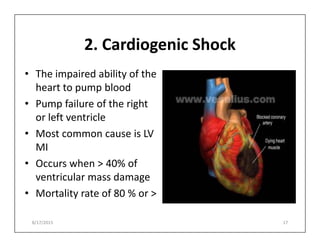
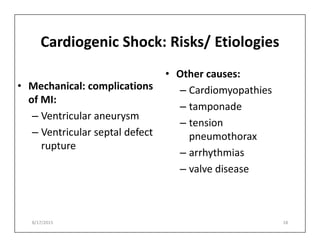
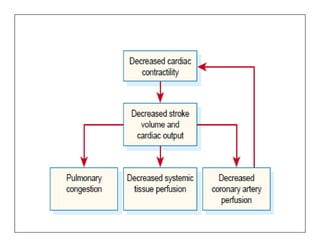
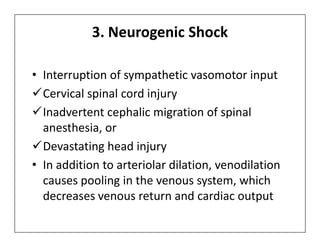
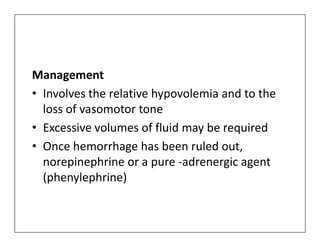
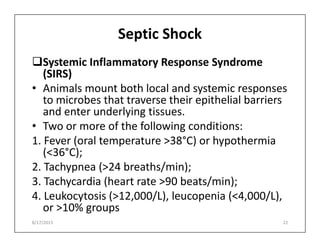
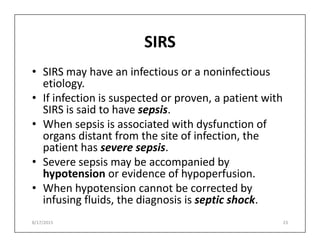
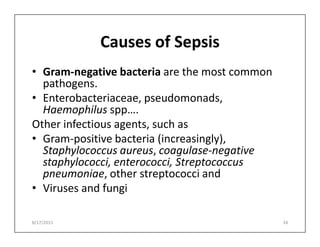
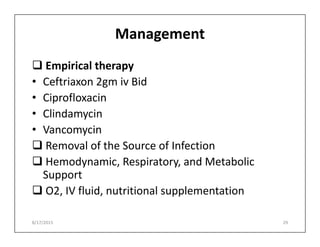
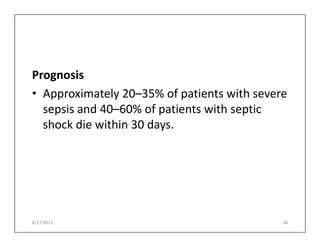
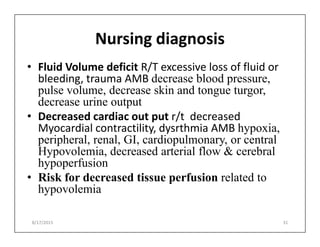
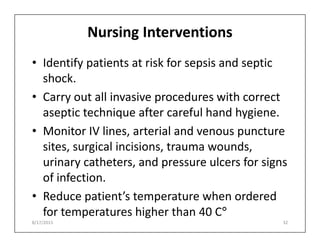
The document discusses shock, a critical condition characterized by inadequate blood circulation preventing essential oxygen and nutrient delivery to body cells. It outlines various types of shock such as hypovolemic, cardiogenic, neurogenic, and septic shock, along with their pathophysiology, clinical manifestations, and management strategies. Additionally, it emphasizes nursing diagnoses and interventions necessary for patients at risk of sepsis and shock-related complications.