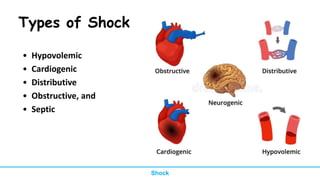
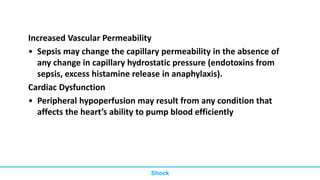
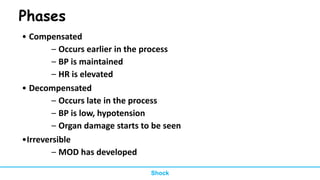
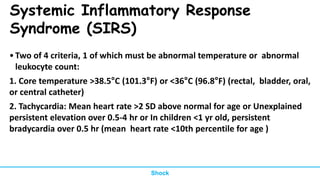
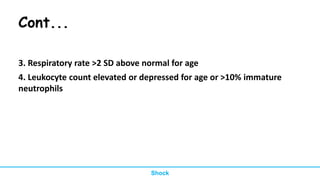
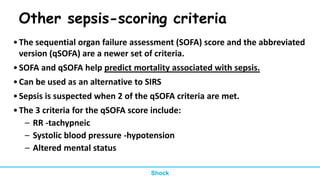
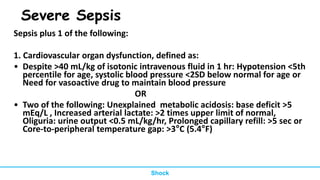
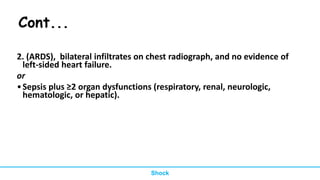
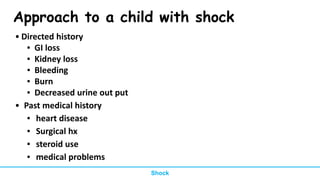
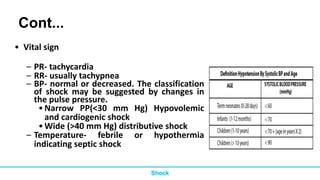
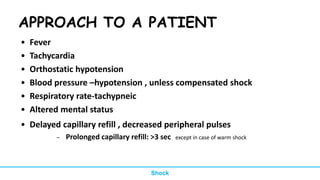
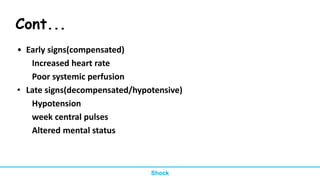
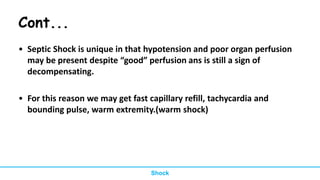
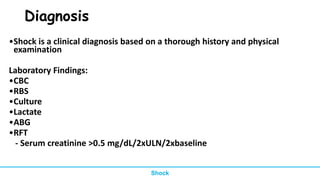
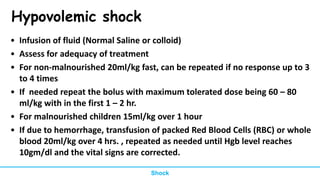
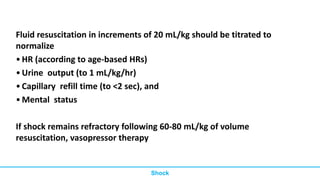
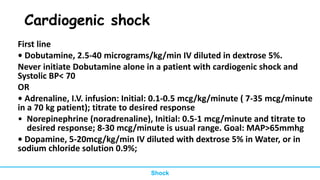
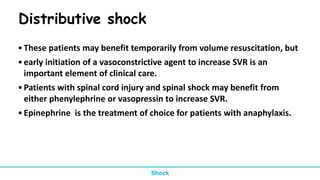
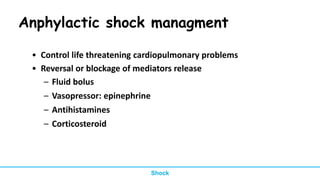
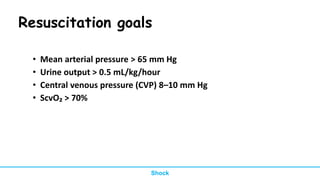
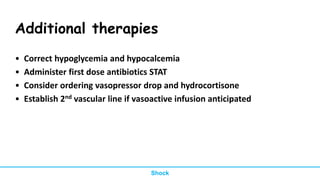
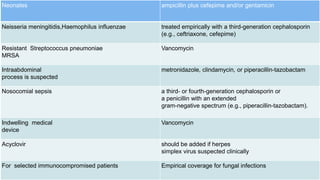
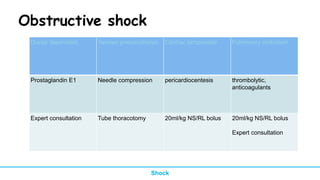
The document provides a comprehensive overview of pediatric shock, detailing its definition, types, pathophysiology, diagnostic approach, and management strategies. It discusses various types of shock, including hypovolemic, cardiogenic, distributive, obstructive, and septic shock, along with their causes and unique features. Management approaches are explored for each type of shock, emphasizing fluid resuscitation, monitoring, oxygenation, and specific treatments for underlying conditions.