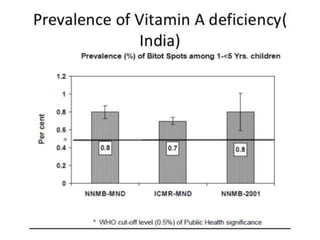
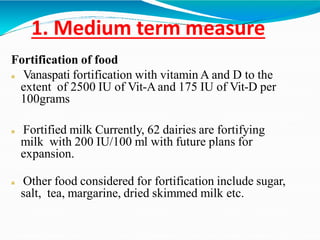
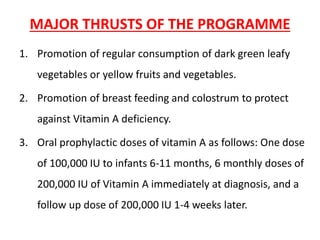
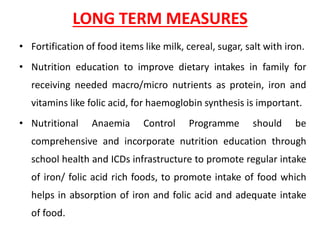
The document discusses India's Vitamin A Prophylaxis Programme launched in 1970. The goals were to eliminate vitamin A deficiency as a public health problem and reduce associated conditions like Bitot's spot and night blindness. Initially, children aged 2-6 years received biannual doses of vitamin A. Starting in 1992, the strategy shifted to providing children aged 9 months to 3 years with 5 mega doses of vitamin A orally to eliminate nutritional blindness and other deficiencies. Food fortification and nutrition education were also emphasized as long term measures to combat vitamin A deficiency.