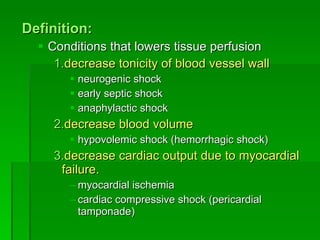
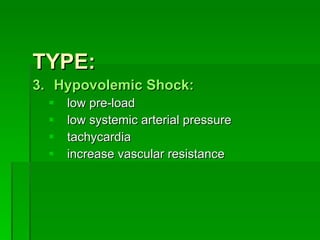
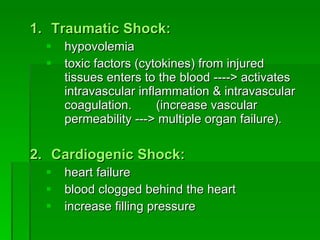
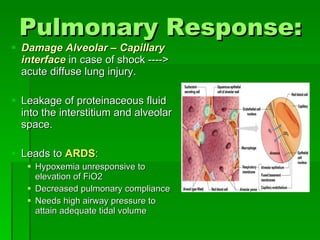
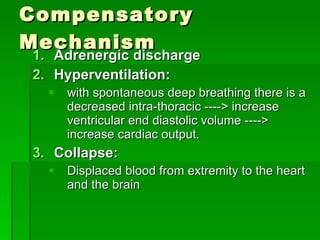
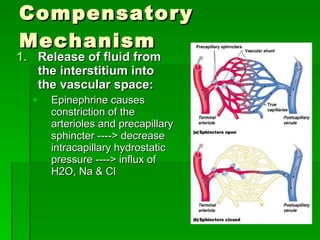
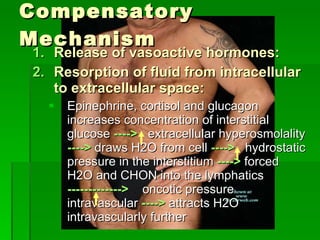
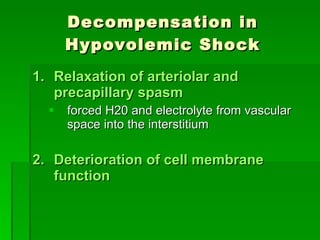
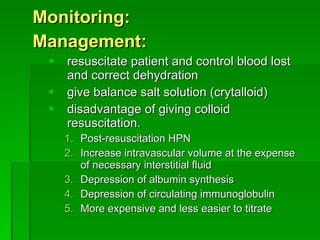
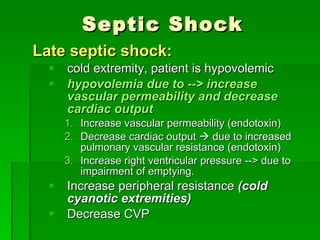
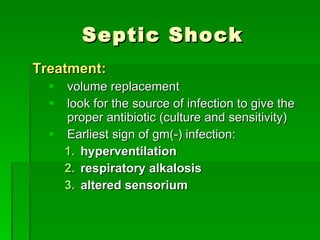
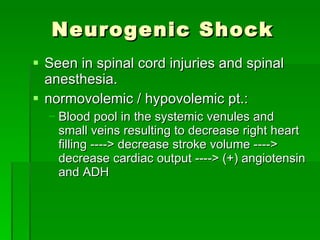
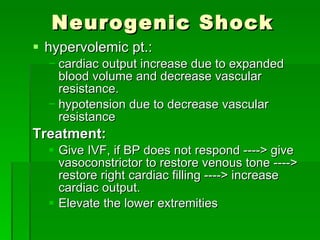
There are several types of shock that result from conditions that lower tissue perfusion and decrease the tonicity of blood vessels. These include hypovolemic, traumatic, cardiogenic, cardiac compressive, septic, and neurogenic shock. The pathophysiology involves decreased tissue perfusion and oxygen delivery leading to cellular changes, dysfunction, and death if not addressed. Management involves identifying the type of shock and treating the underlying cause while resuscitating the patient with fluids to restore intravascular volume and hemodynamics.