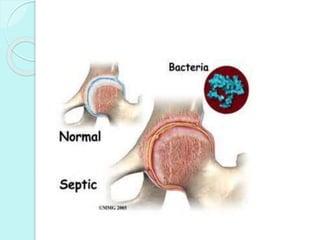
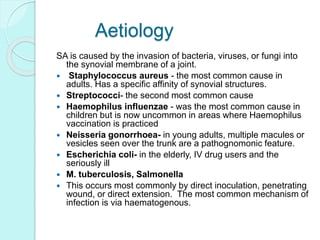
Septicarthritis is an inflammation of the synovial membrane of a joint caused by bacterial, viral, or fungal infection. Staphylococcus aureus is the most common cause in adults. Symptoms include severe pain, swelling, warmth and limited range of motion in the infected joint. Diagnosis involves joint fluid analysis showing purulent material and inflammatory markers. Treatment requires antibiotics, drainage of pus, and sometimes surgery. Without rapid treatment, joint destruction and long-term disability can occur.





![REFERENCES
Septic Arthritis Aspiration Techniques
and Indications for Surgery at
Medscape. Author: Nadera Sweiss.
Updated: Feb 7, 2012
Prosthetic Joint Infectious Arthritis:
Infections of Joints and Bones: Merck
Manual Professional [Internet]. [cited
2010 Feb 16];Available
Klippel, J.H., et al. Primer on the
Rheumatic Diseases. New York:
Springer, 2008.](https://image.slidesharecdn.com/arthritis-150909111055-lva1-app6892/85/Septic-Arthritis-39-320.jpg)