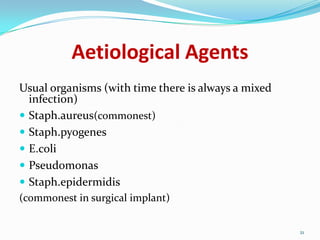
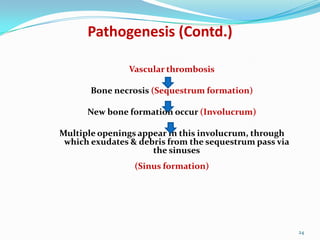
Osteomyelitis is an inflammatory process of bone caused by bacterial infection. It can be acute, subacute, or chronic depending on duration. The most common causative organism is Staphylococcus aureus. Acute osteomyelitis typically affects children and causes fever, pain, and swelling near the infected bone. Chronic osteomyelitis results from inadequate treatment of acute osteomyelitis and causes persistent infection, bone necrosis, and sinus tract formation. Surgical debridement along with long-term antibiotics is usually required to treat chronic osteomyelitis. Rehabilitation focuses on restoring range of motion and strength through exercises.






















![Treatment - Antibiotics
-
Chronic infection is seldom
eradicated by antibiotics alone.
-
Antibiotic (IV route) is given for 10
days prior to surgery.
-
Bactericidal drugs are important
to:
a) Stop the spread of infection to
healthy bone
b) Control acute flares
-
After the major debridement
surgery, antibiotic is
continued for another 6 weeks
(min) but usually >3months.
[treat until inflammatory
parameters (ESR) are normal]
-
Antibiotics used in treating
chronic osteomyelitis
(Fusidic acid, Clindamycin,
Cefazolin)
27](https://image.slidesharecdn.com/osteomyelitis-130928124500-phpapp01-140129083843-phpapp02/85/Osteomyelitis-27-320.jpg)








