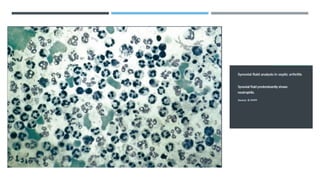
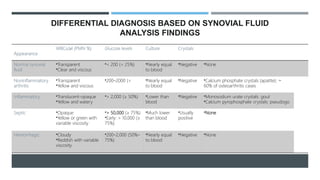
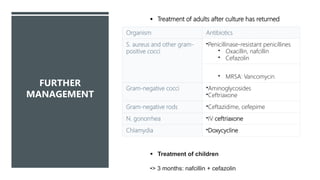
Septic (infectious) arthritis is a bacterial infection of the joint space that can occur via bloodstream spread, local extension from a wound or trauma, or iatrogenically. It presents with an acutely swollen, painful and stiff joint along with fever. Diagnosis requires prompt arthrocentesis to analyze synovial fluid for signs of infection like white blood cell count over 50,000/μL and culture the fluid to identify the bacteria. Treatment involves immediate antibiotics as well as surgical drainage and debridement if needed to prevent joint damage.

![SUBTYPES AND
VARIANTS
Prosthetic joint infection
Etiology [4]
Early onset (< 3 months of placement); most commonly S. aureus
Delayed onset (3–12 months of placement); particularly S. epidermidis
most commonly S. aureus
Clinical findings
Usually prolonged, low-grade course
Can present acutely](https://image.slidesharecdn.com/septicarthritis-200704234340/85/Septic-arthritis-6-320.jpg)