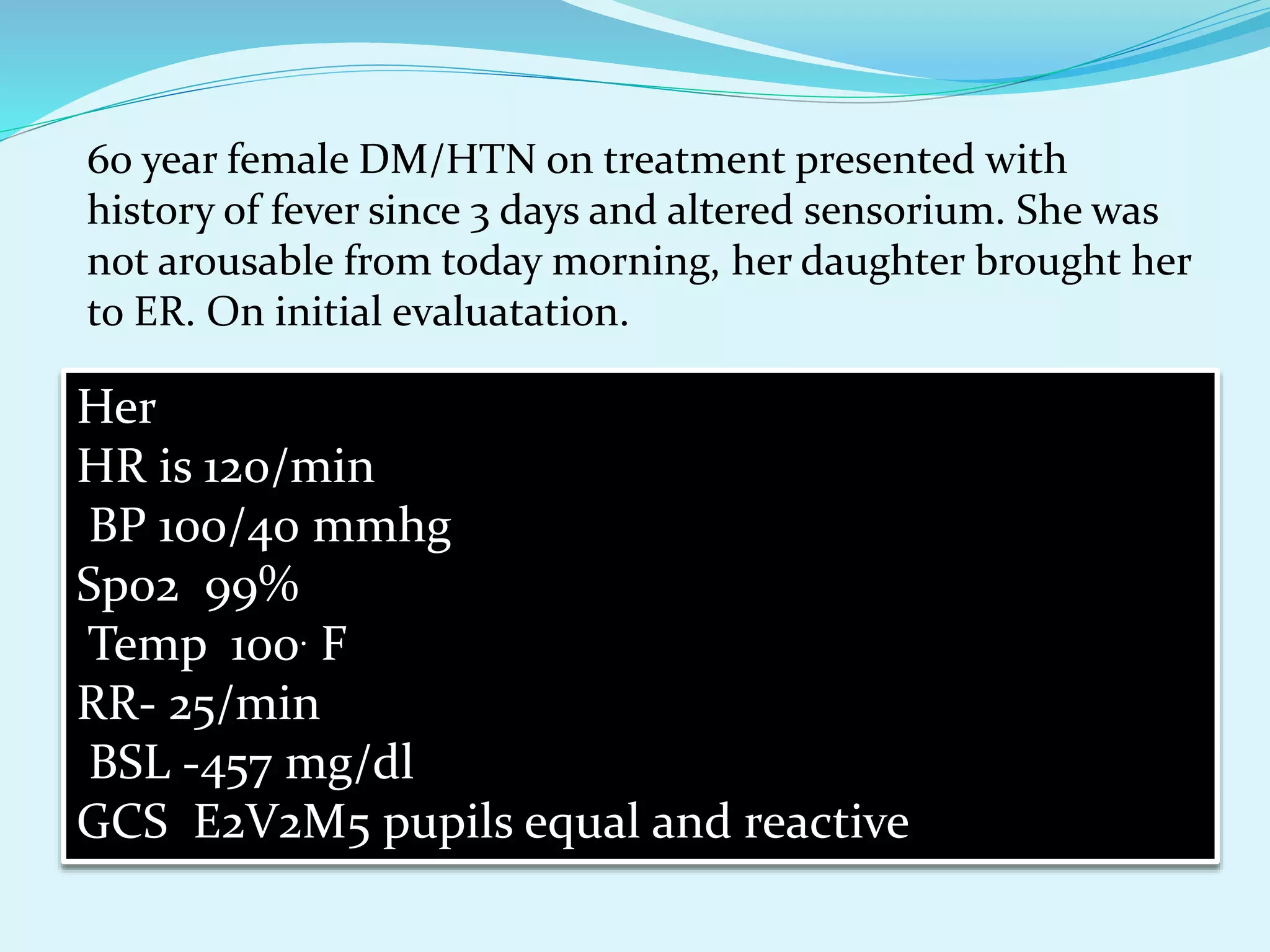
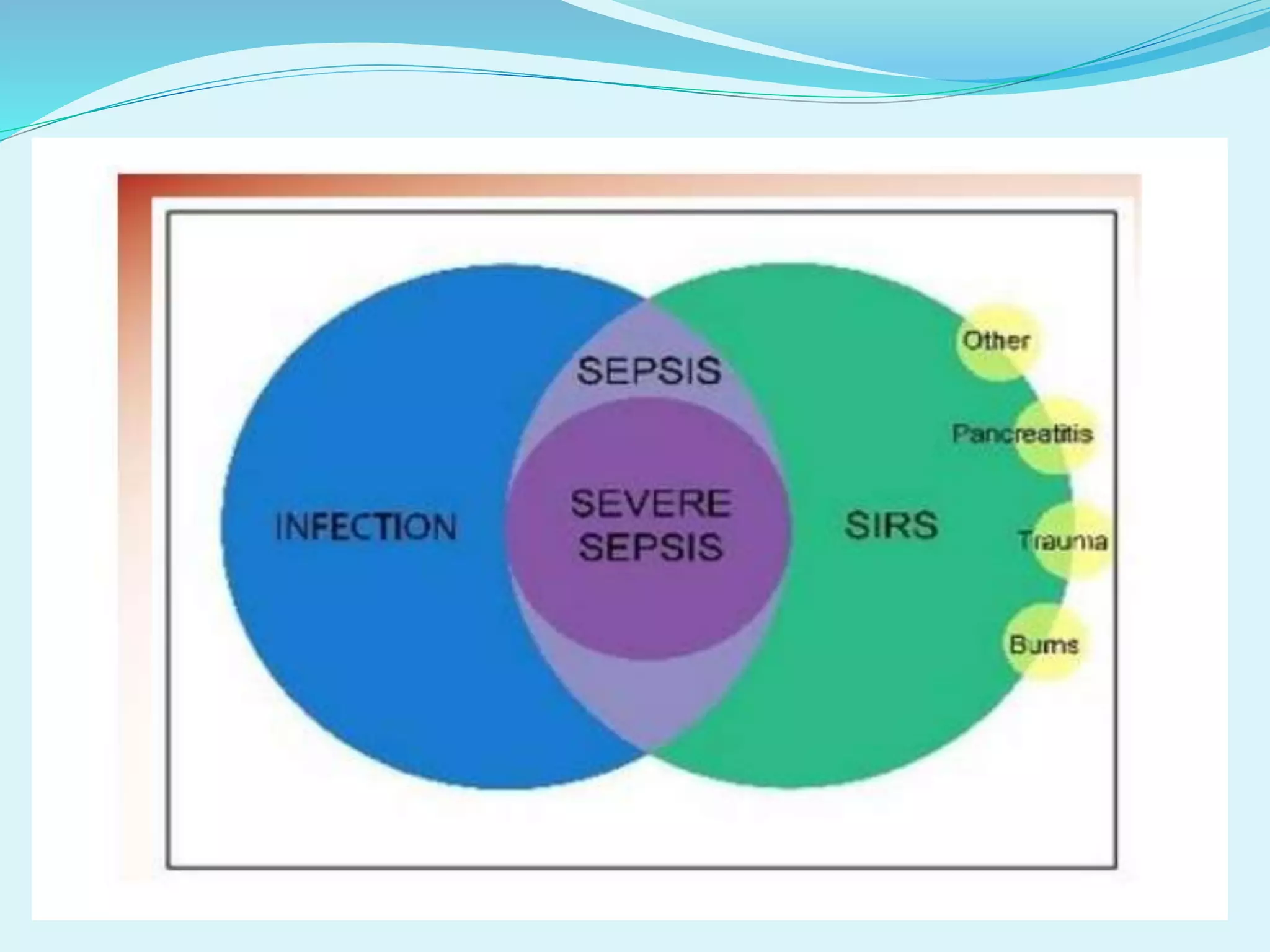
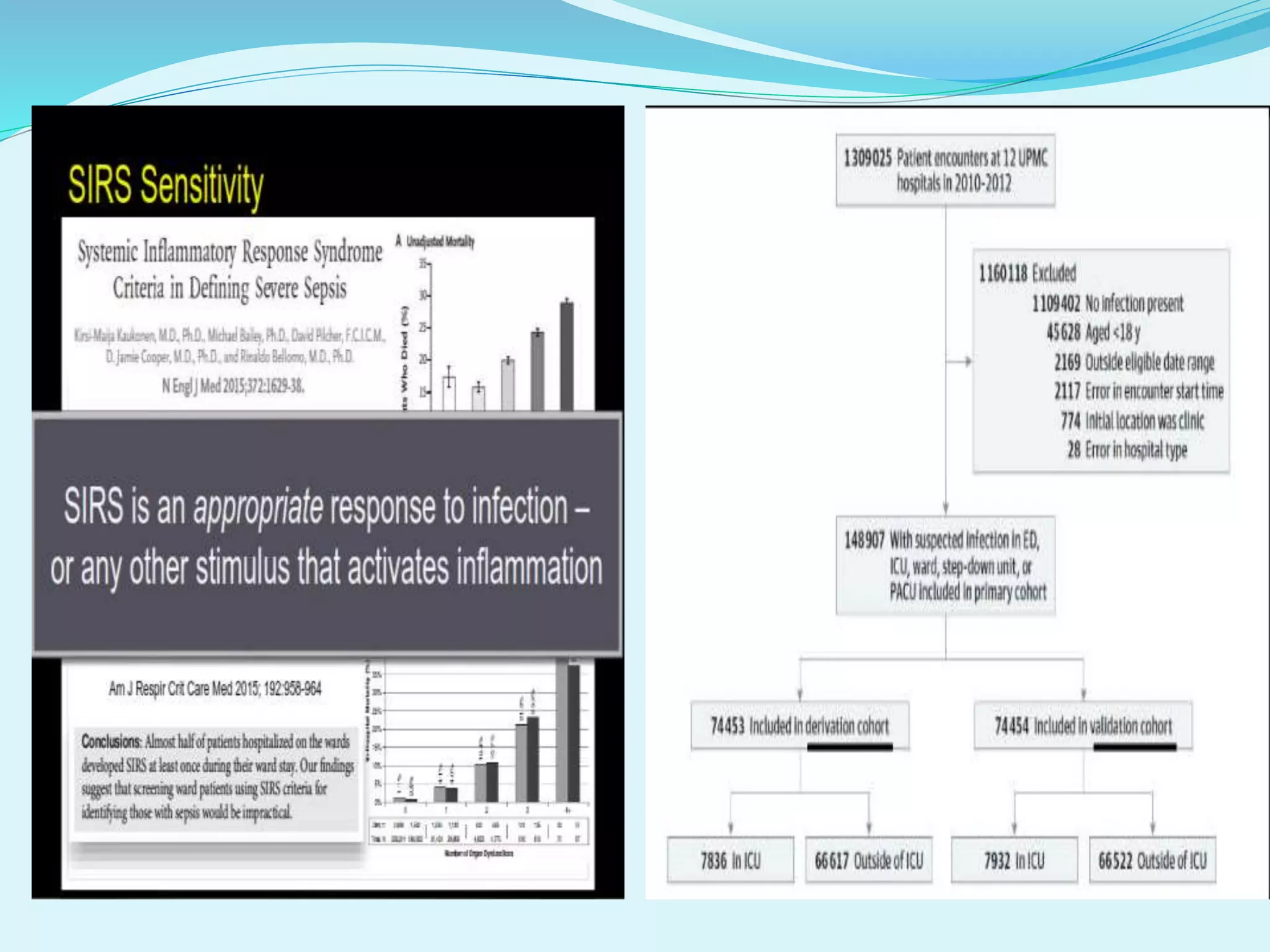
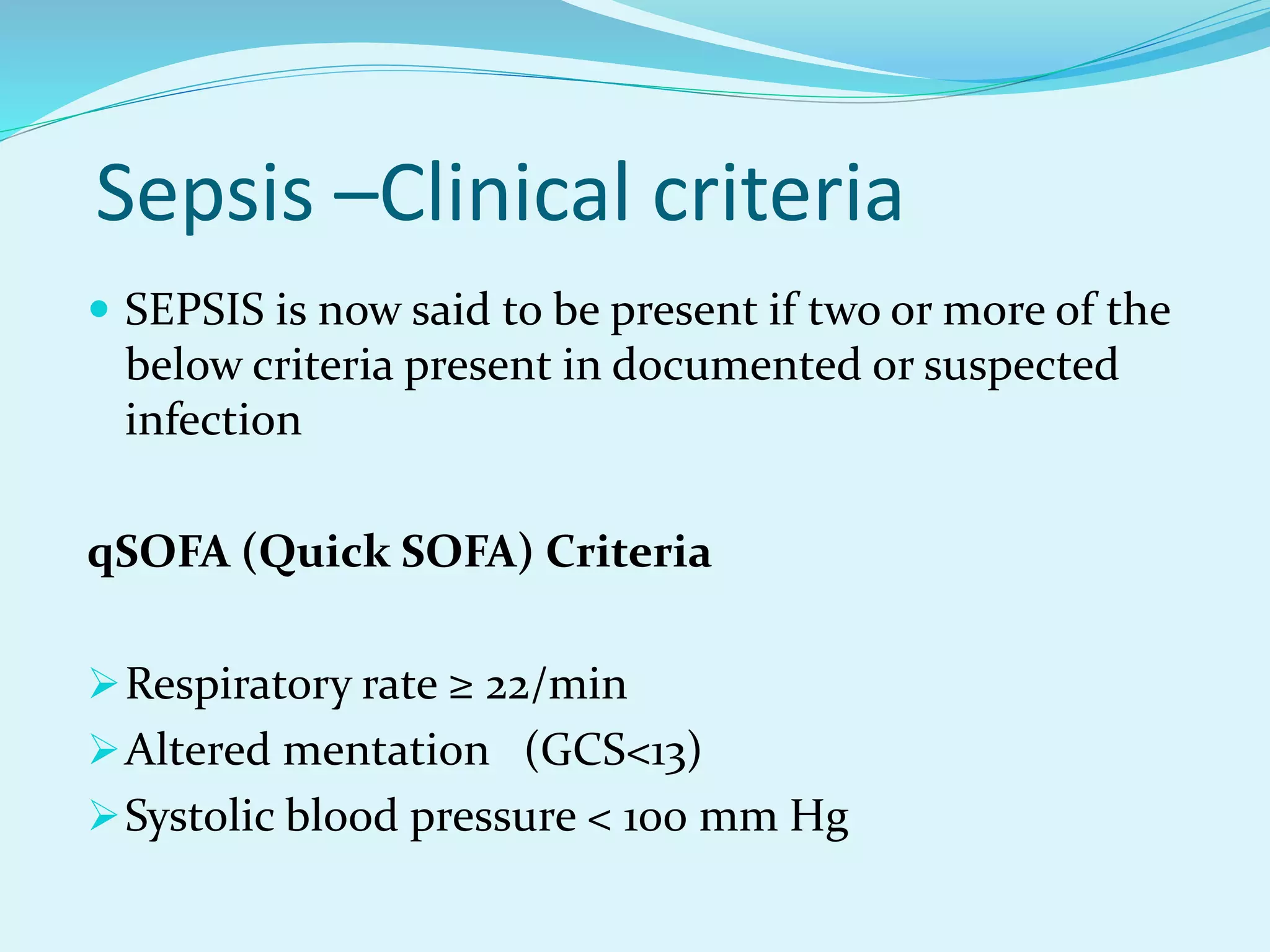
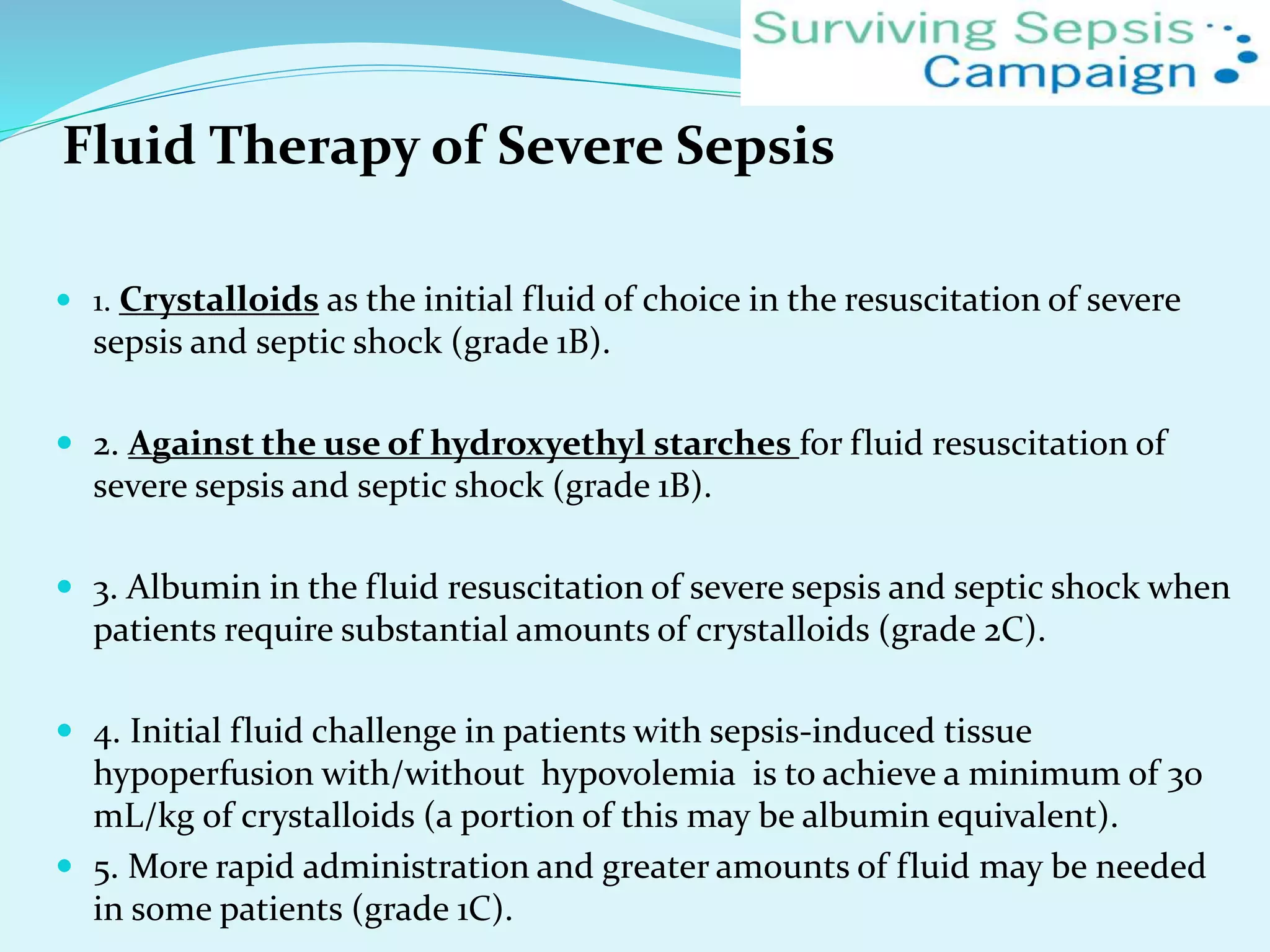
A 60-year-old female with diabetes and hypertension presented with altered mental status and fever for 3 days. On examination, she had a high heart rate, low blood pressure, high respiratory rate, and high blood glucose. Initial lab work showed high lactate, low platelets, and signs of infection on urine and blood tests. This patient is showing signs of sepsis such as altered mental status, hypotension, and elevated lactate. The initial response should be rapid fluid resuscitation with crystalloids, broad-spectrum antibiotics, and vasopressors if needed to maintain blood pressure. Close monitoring and treatment based on sepsis guidelines is needed in the first critical hours to prevent further organ dysfunction.