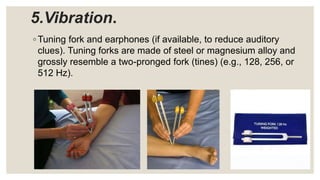
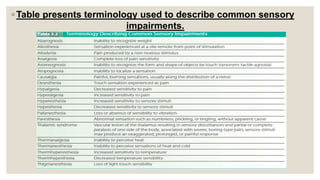
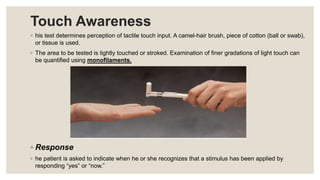
This document provides information about screening and examining sensory function. It discusses preparing the testing environment and equipment needed, including items to test pain, temperature, light touch, vibration, stereognosis, and two-point discrimination. The order of testing sensations from superficial to deep is described. For each test, data on the modality, involvement, severity, boundaries, and impact will be collected. Proper administration techniques are outlined, such as applying stimuli randomly and accounting for skin conditions. Terminology for describing sensory impairments is also provided.