The document summarizes the somatosensory system. It discusses:
1) The sensory nervous system processes sensory information through sensory neurons, pathways, and brain areas.
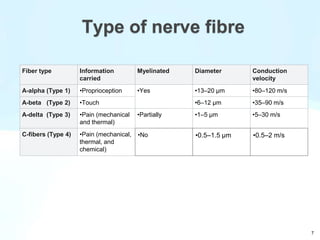
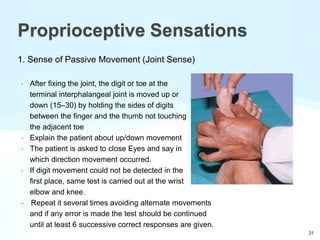
2) There are different sensory modalities including touch, temperature, pain, and proprioception.
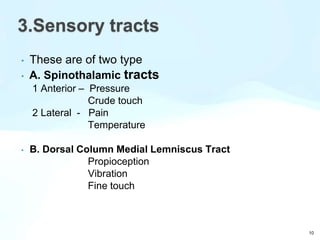
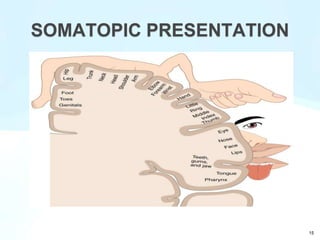
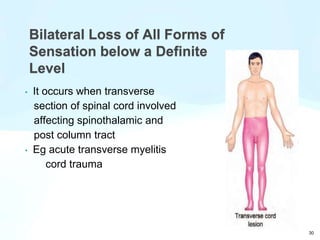
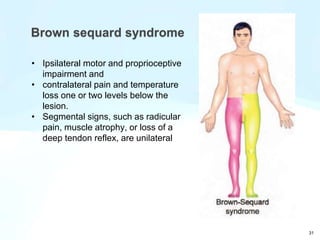
3) Sensory pathways include cutaneous innervation, dermatomes, tracts like the spinothalamic and dorsal column medial lemniscus tracts, and sensory areas in the brain.
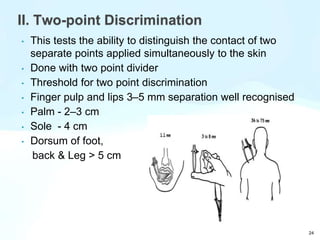
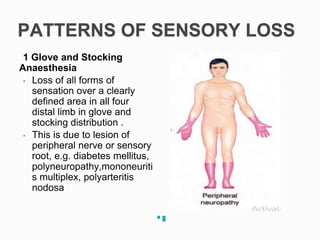
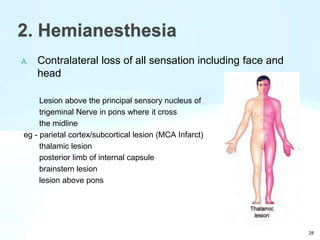
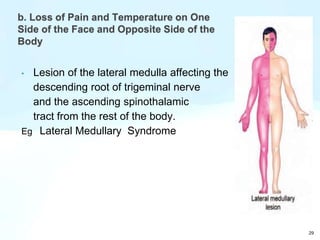
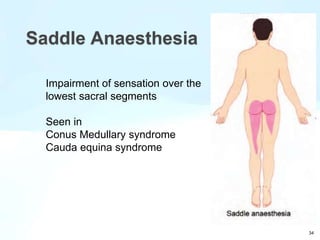
4) Examination of sensation tests modalities like pain, temperature, vibration and cortical sensations to localize lesions. Common patterns of sensory loss include glove/stocking, hemianaesthesia, and spinal cord lesions.