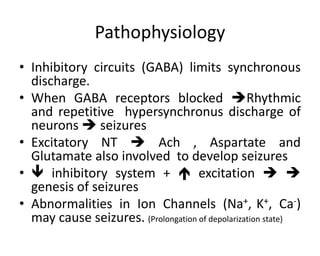
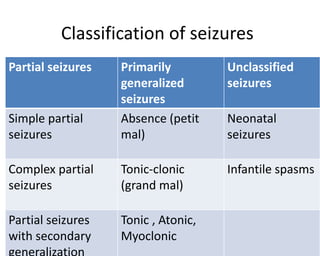
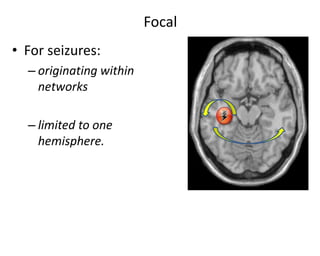
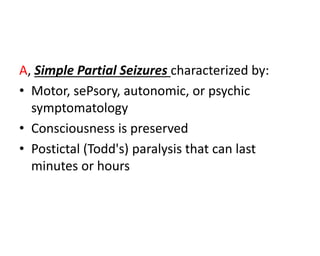
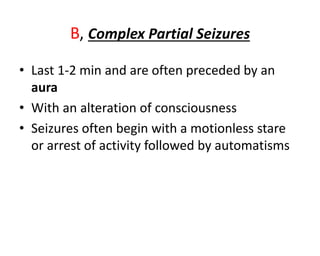
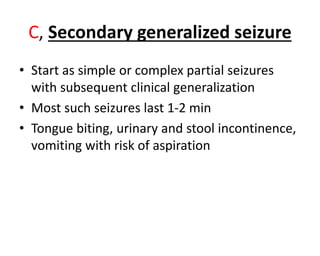
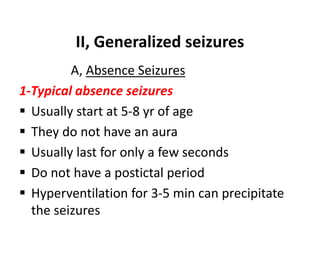
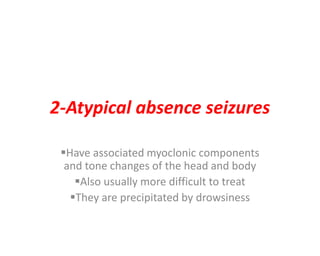
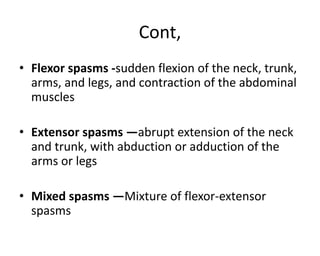
1) Seizures are caused by abnormal excessive synchronous firing of neurons in the brain. They can be classified as partial or generalized seizures. Status epilepticus refers to continuous or recurrent seizures without regaining consciousness.
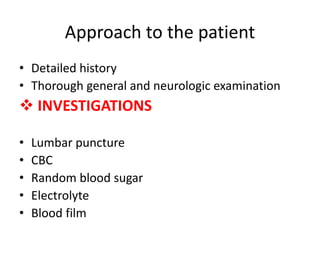
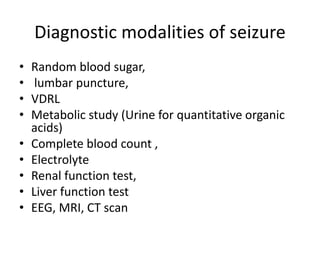
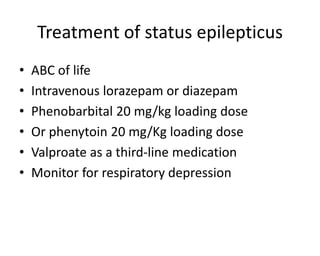
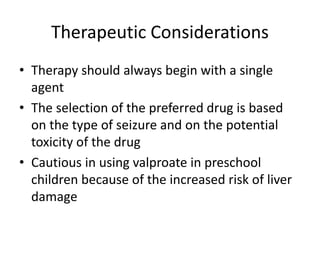
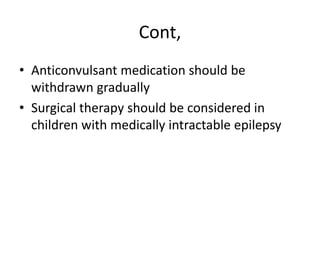
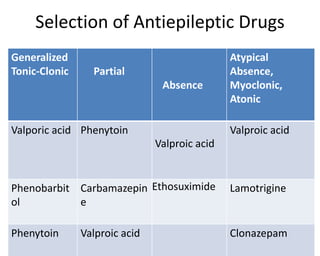
2) Evaluation of seizures involves a detailed history, exam, and tests like EEG, MRI and bloodwork to identify underlying causes. Treatment depends on seizure type and includes antiepileptic drugs, adrenocorticotropic hormone for infantile spasms, and surgery for refractory cases.
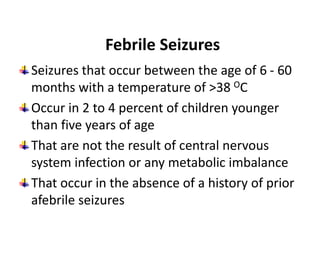
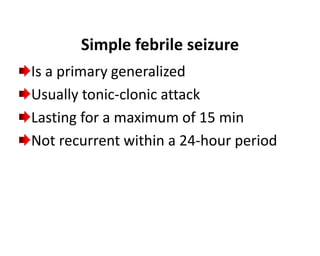
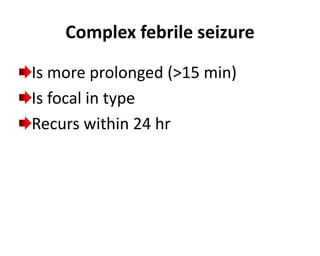
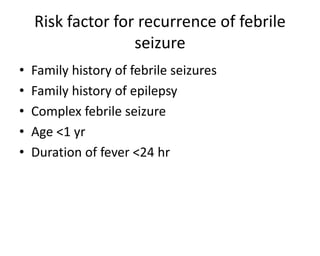
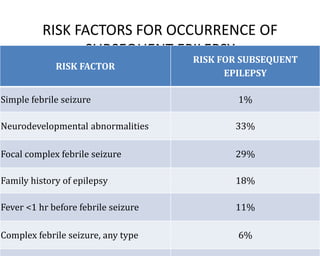
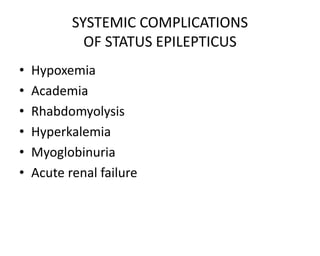
3) Febrile seizures are common in young children and usually resolve without complications, but complex febrile seizures and other risk factors increase risk of developing epilepsy later in life. Proper management of status epile