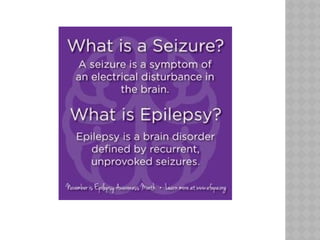
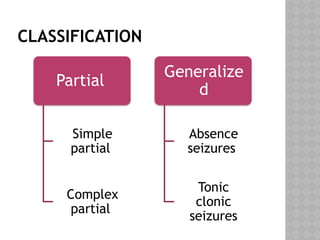
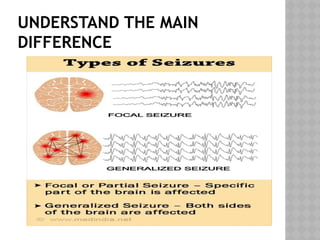
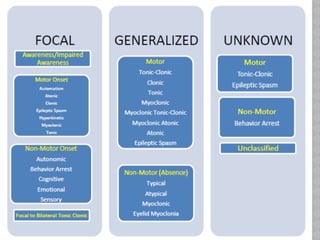
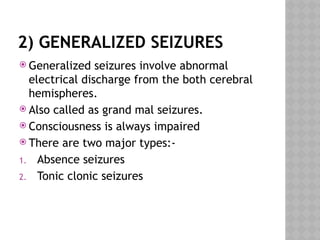
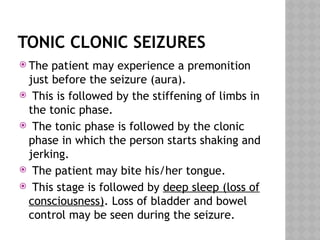
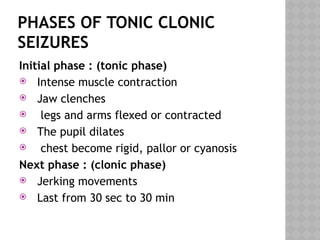
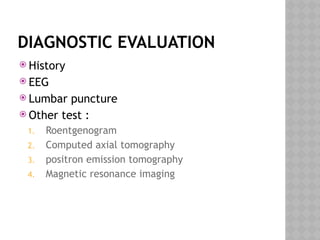
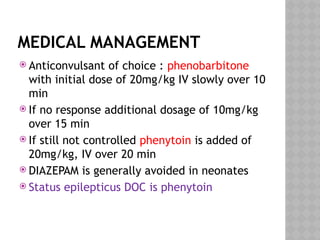
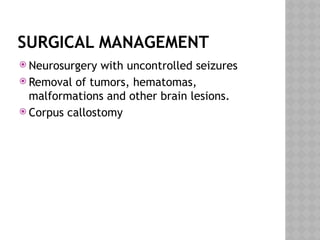
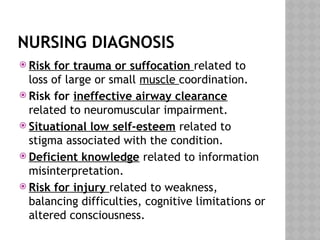
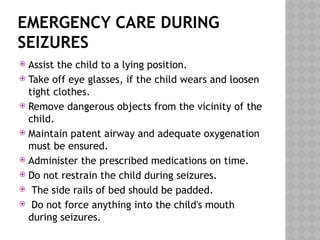
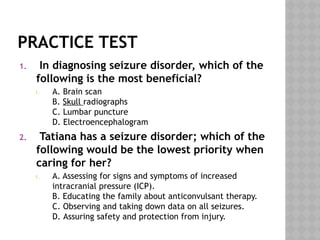
The document provides a detailed overview of seizure disorders, differentiating between epilepsy, seizures, and convulsions, along with their classifications such as partial and generalized seizures. It describes the specific characteristics, diagnostic approaches, medical and surgical management, nursing assessments, and emergency protocols for handling seizures, particularly in children. Additionally, it emphasizes the importance of education for caregivers regarding the condition and proper care during seizures.