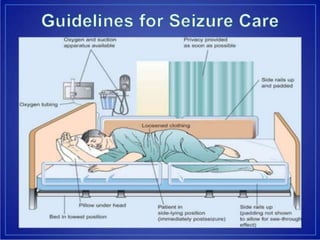
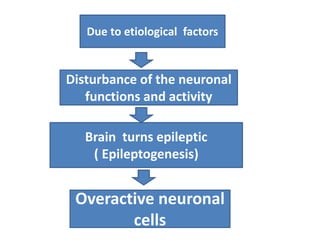
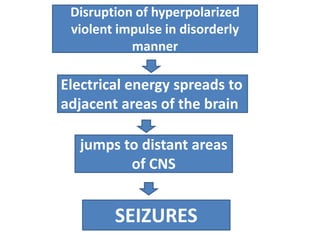
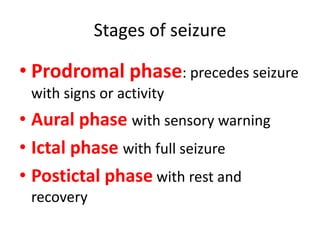
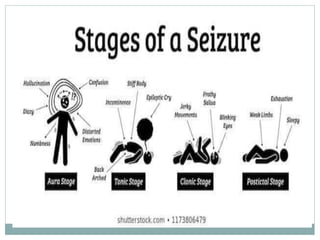
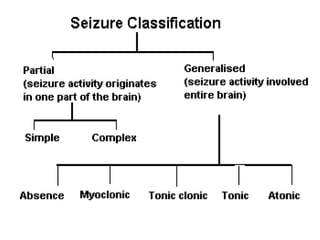
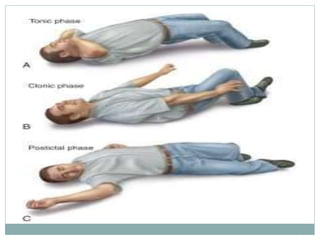
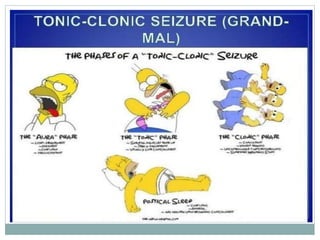
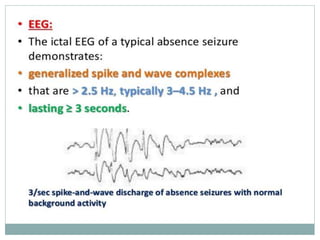
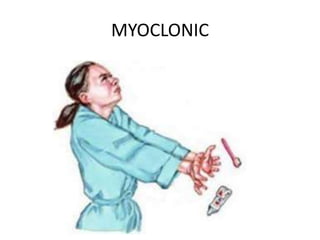
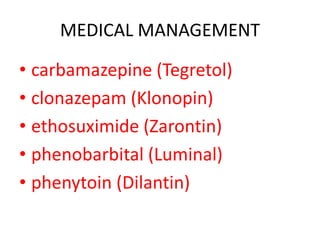
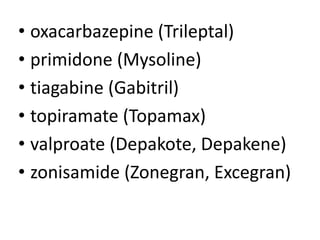
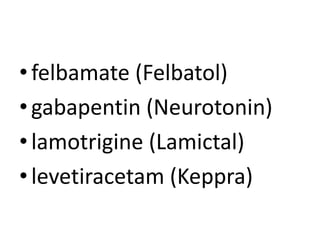
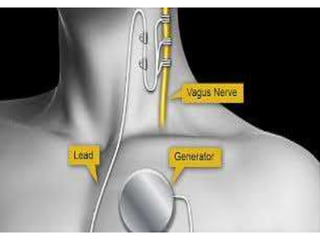
This document provides information on seizures and epilepsy. It defines seizures as uncontrolled electrical discharges in the brain that interrupt normal function. Epilepsy is defined as a recurrent seizure disorder caused by abnormal brain activity. Seizures can be caused by genetic, developmental, infectious, or environmental factors. The stages of a seizure are the prodromal, ictal, and postictal phases. Seizures are classified as partial or generalized and have different clinical manifestations depending on the affected brain region. Diagnosis involves a history, physical exam, EEG, and sometimes CT/MRI. Treatment includes anti-seizure medications, dietary therapies, surgery, and nursing care during and after seizures to prevent injury.


![Nursing Care During a Seizure
• Provide privacy and protect the patient from
curious on-lookers. (The patient who has an
aura [warning of an impending seizure] may
have time to seek a safe, private place.)
• Ease the patient to the floor, if possible.
• Protect the head with a pad to prevent injury
(from striking a hard surface).
• Loosen constrictive clothing.](https://image.slidesharecdn.com/seizures-210210103306/85/Seizures-40-320.jpg)