Convulsive disorders are neurological conditions characterized by recurrent, involuntary seizures caused by abnormal electrical activity in the brain. Common types of convulsive disorders include epilepsy, febrile seizures in children, and status epilepticus, which requires immediate medical attention.
Approximately 5% to 10% of children will experience at least one seizure by the age of 16.
The prevalence of epilepsy in children is estimated to be around 0.5% to 1%.
Febrile seizures occur in about 2% to 5% of children aged 6 months to 5 years, typically triggered by a rapid rise in fever.
Status Epilepticus occurs in about 0.2% to 0.5% of children with epilepsy.
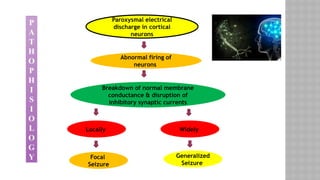
Seizures: Seizures are sudden, uncontrolled electrical disturbances in the brain that can cause changes in behavior, movements, feelings, or consciousness.
Convulsions: Convulsions refer to the physical manifestations of a seizure, characterized by violent, uncontrolled shaking or jerking movements of the body. Convulsions can occur in various types of seizures.
Febrile Seizures: Febrile Seizures are convulsions triggered by fever, typically in children aged 6 months to 5 years, without an underlying neurological cause.
Epilepsy: Epilepsy is a chronic neurological disorder characterized by recurrent, unprovoked paroxysmal seizures. It can result from a variety of underlying causes, including genetic factors, brain injuries, or structural abnormalities in the brain.
Status Epilepticus: Status epilepticus is a medical emergency defined as a prolonged seizure lasting more than 5 minutes or a series of seizures without recovery between them.
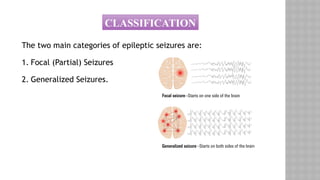
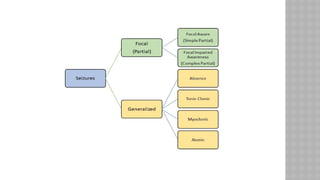
The two main categories of epileptic seizures are:
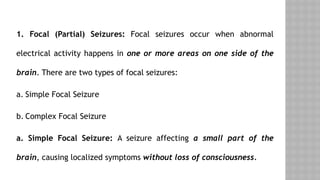
Focal (Partial) Seizures
Generalized Seizures.