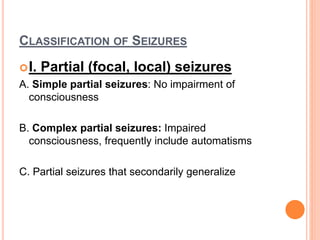
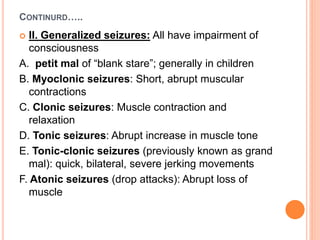
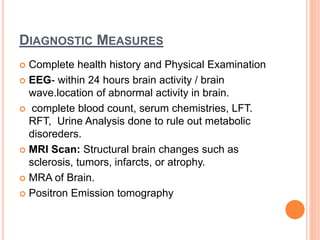
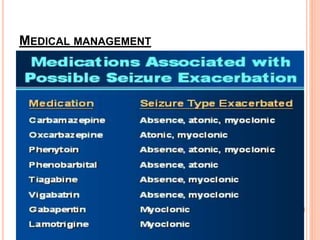
Seizures are episodes of abnormal brain activity resulting from excessive neuronal discharge. Epilepsy is characterized by recurrent seizures and is caused by various factors like brain tumors, genetic predisposition, trauma and infections. Seizures can be classified as partial or generalized based on the area of brain involved. Diagnostic tests include EEG, MRI and blood tests. Treatment involves medications, surgery, vagus nerve stimulation or lifestyle modifications. Nursing care focuses on safety during seizures and education about managing the condition.
![ETIOLOGY
*About half the cases of epilepsy are
unknown.
*Possible causes include the following:
Disorder of the Brain: Tumor, Abscess,
Atrioventricular malformation [AVM], aneurysm, or
hematoma
Genetic /Family History.
Congenital Abnormalities.
Perinatal Factors:- Birth trauma and asphyxia
neonatorum](https://image.slidesharecdn.com/seizure-200125054207/85/Seizure-and-nursing-care-3-320.jpg)