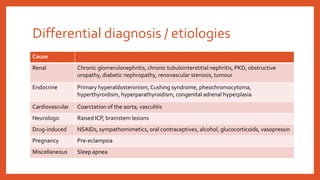
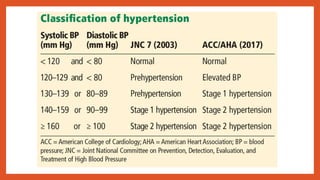
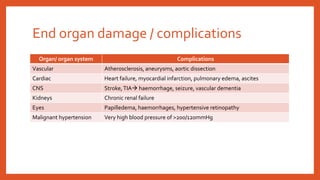
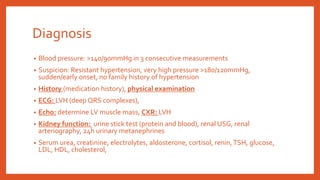
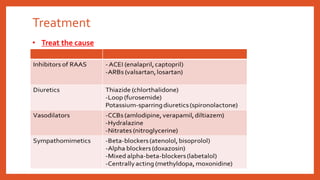
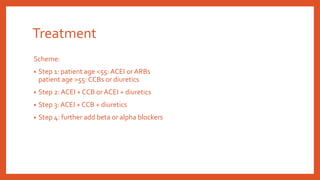
The document discusses the differential diagnosis and treatment of elevated systemic arterial blood pressure, which accounts for 10-20% of hypertensive patients. It covers various etiologies, including renal, endocrine, cardiovascular, neurologic, and drug-induced causes, as well as clinical manifestations, complications, and diagnostic measures. Treatment strategies are outlined based on patient age and may involve a combination of medications, including ACE inhibitors, calcium channel blockers, and diuretics.