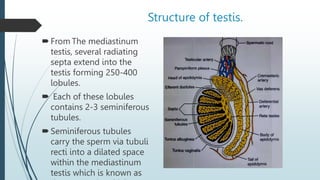
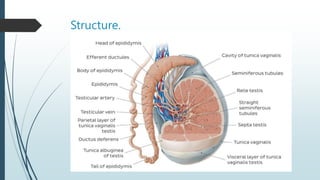
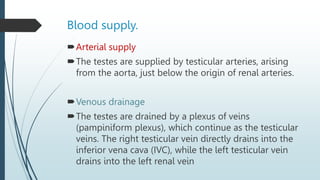
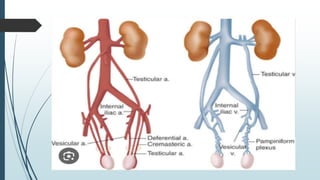
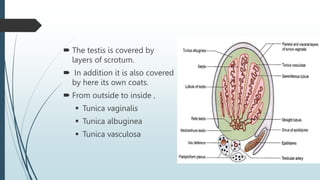
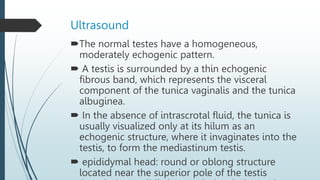
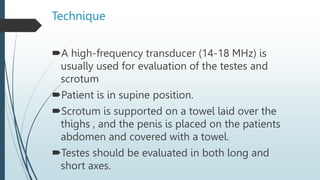
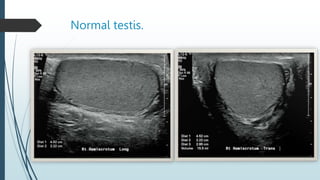
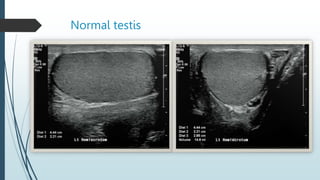
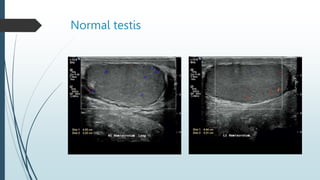
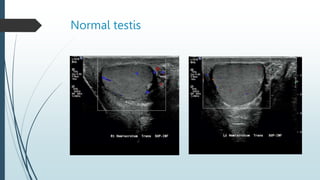
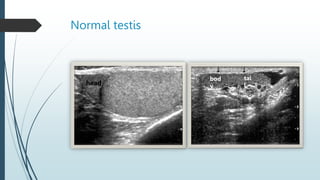
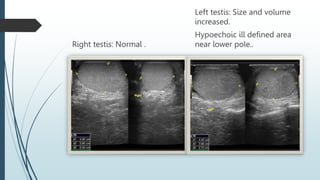
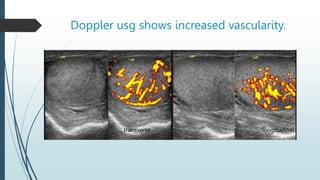
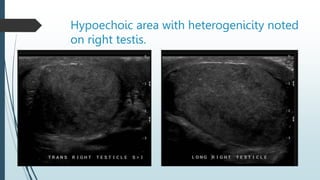
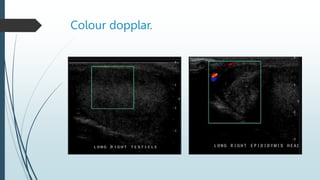
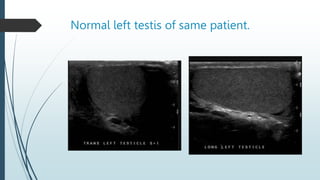
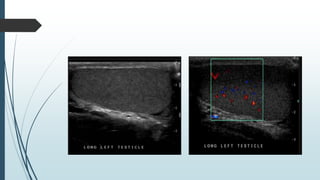
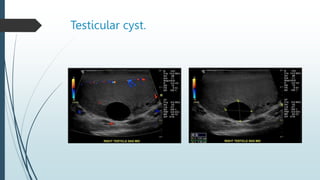
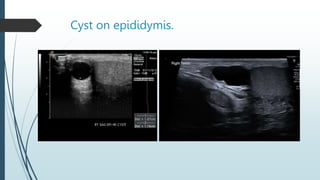
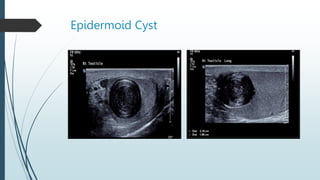
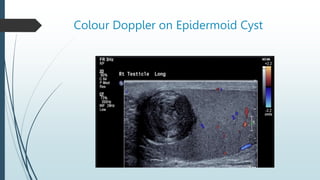
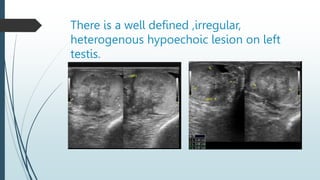
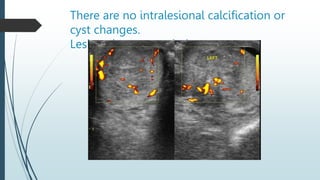
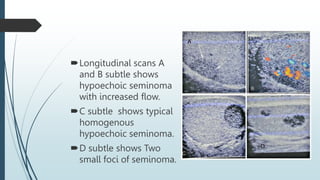
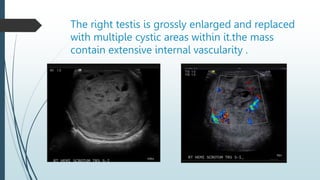
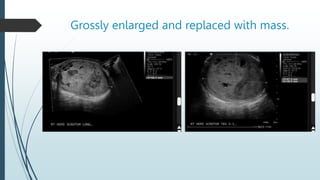
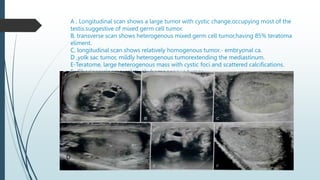
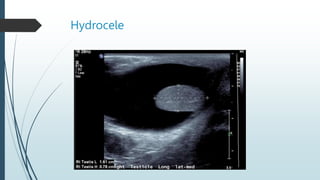
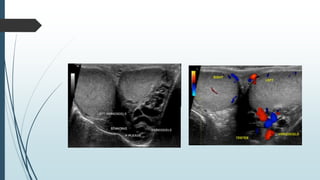
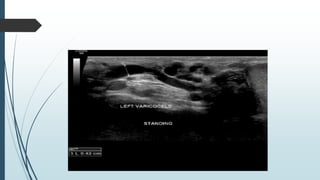
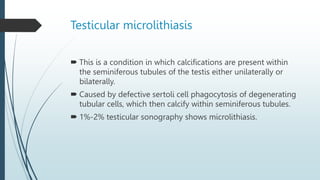
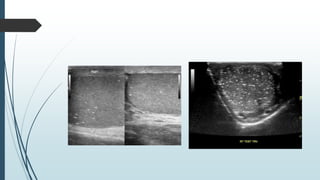
The document summarizes sonographic evaluation of the testis. It describes the normal anatomy and structures of the testis including the seminiferous tubules, mediastinum testis, and epididymis. Common pathologies seen on ultrasound are discussed such as orchitis appearing as diffuse hypoechogenicity and increased vascularity, and torsion seen as swelling and decreased or absent blood flow. Testicular tumors manifest as intratesticular hypoechoic lesions, while cysts are anechoic. The technique of scrotal ultrasound emphasizes using a high-frequency transducer in both longitudinal and transverse planes.