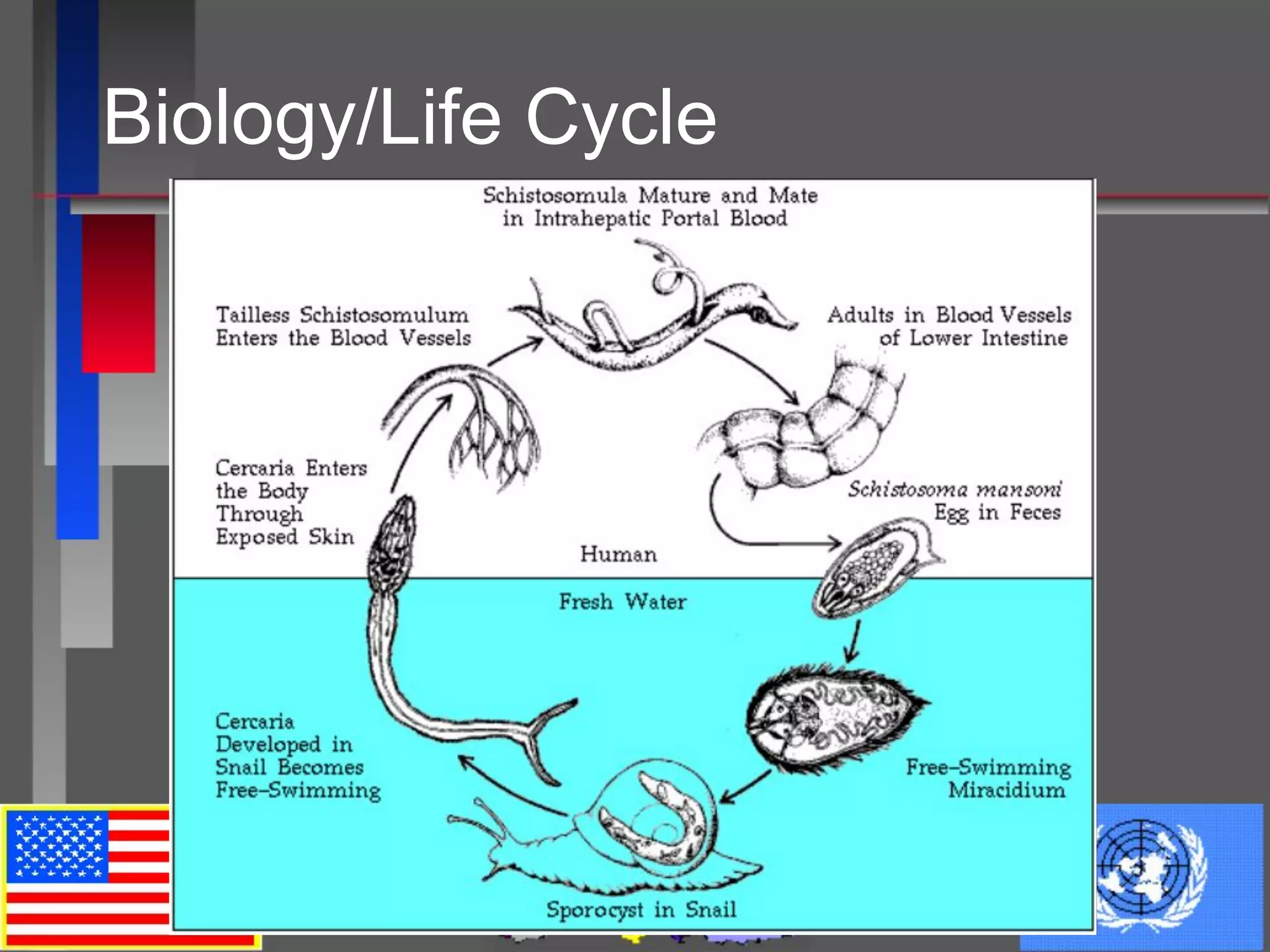
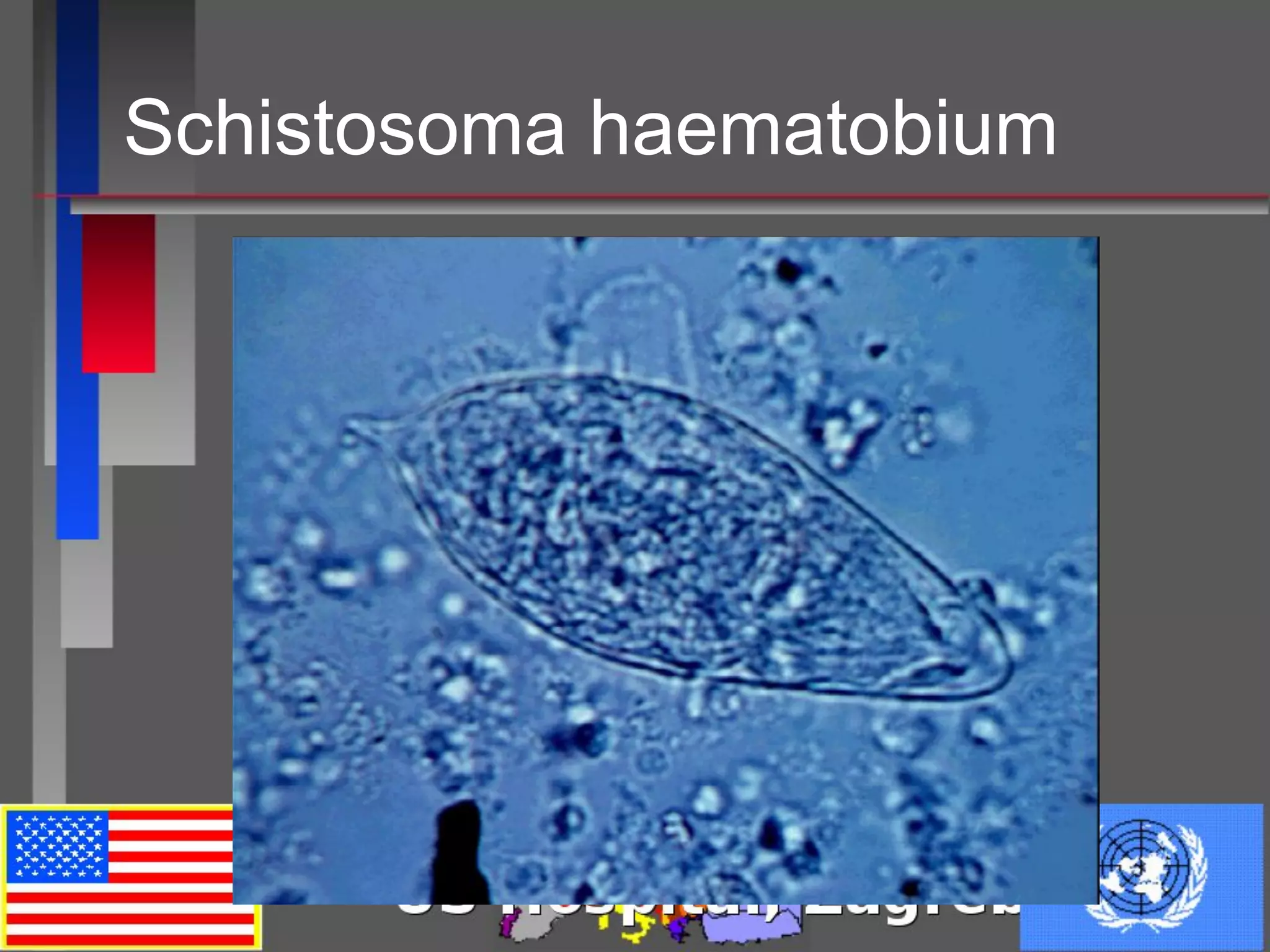
This document discusses a case of Schistosomiasis haematobium in a 25-year-old male from Kenya. Laboratory tests found eggs of S. haematobium in the patient's urine. The document then provides details on the life cycle, epidemiology, clinical manifestations, diagnosis, and treatment of schistosomiasis. Schistosomiasis remains a major public health problem worldwide, with certain areas of Africa and the Philippines having high infection rates. Praziquantel is the treatment of choice.