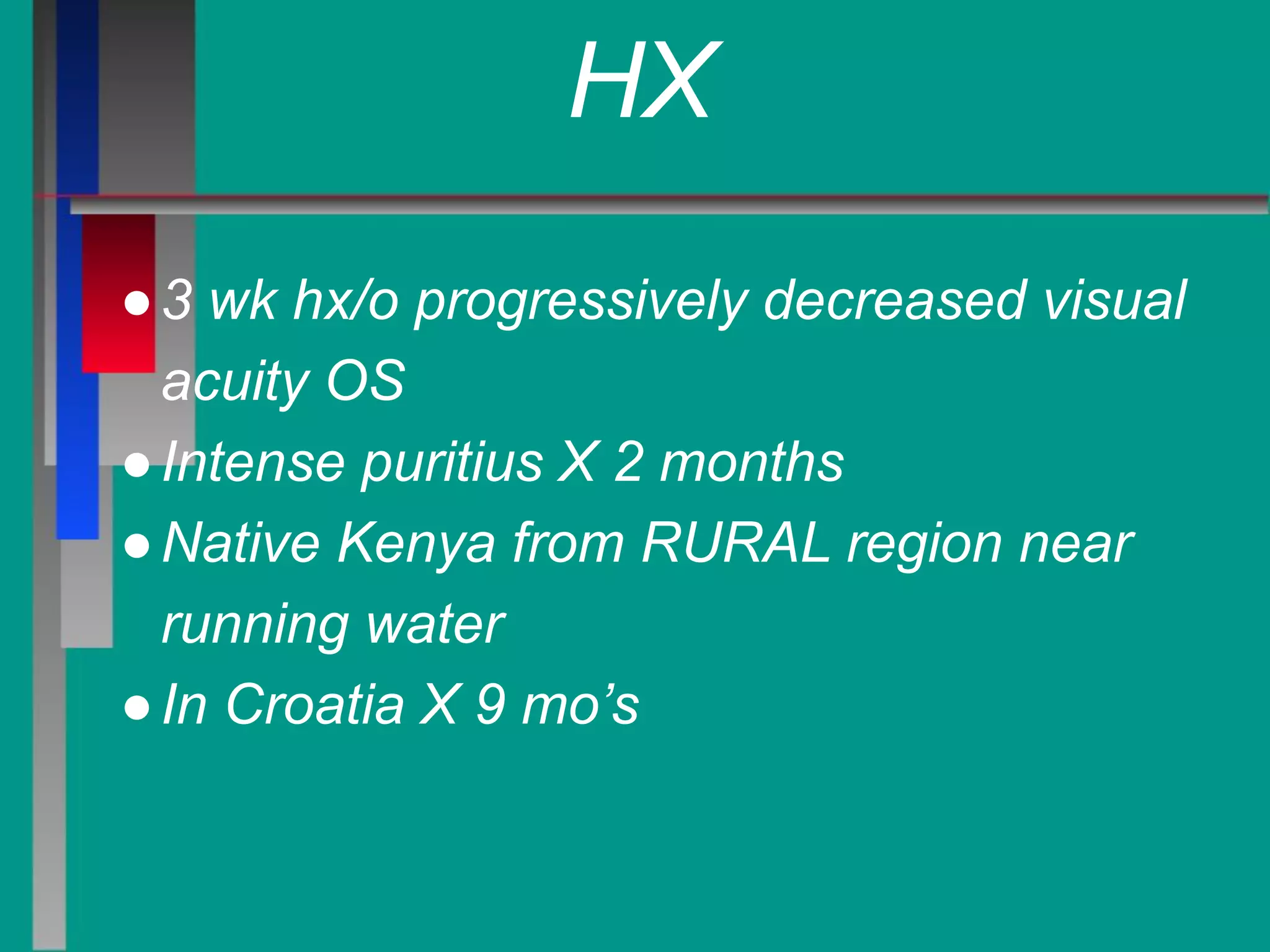
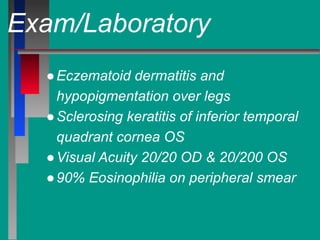
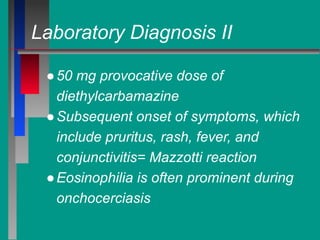
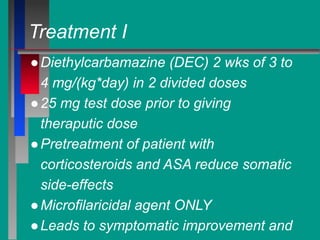
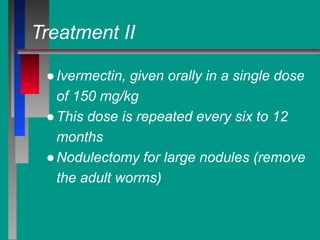
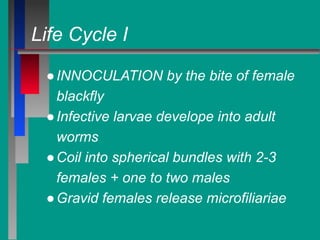
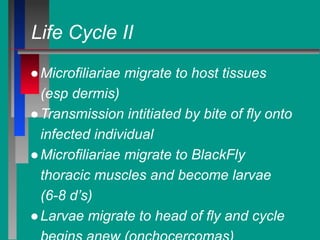
The patient is a native of Kenya who recently spent 9 months in Croatia and presents with progressively decreased vision in the left eye over 3 weeks. Exam finds eczematoid dermatitis and hypopigmentation of the legs with sclerosing keratitis of the left cornea. Labs show 90% eosinophilia. The document discusses onchocerciasis, caused by the filarial nematode Onchocerca volvulus transmitted by blackflies in equatorial Africa and other regions. Clinical manifestations include skin lesions, subcutaneous nodules, and eye involvement that can lead to blindness. Diagnosis involves skin snip biopsy and treatment is diethylcarbamazine or ivermectin