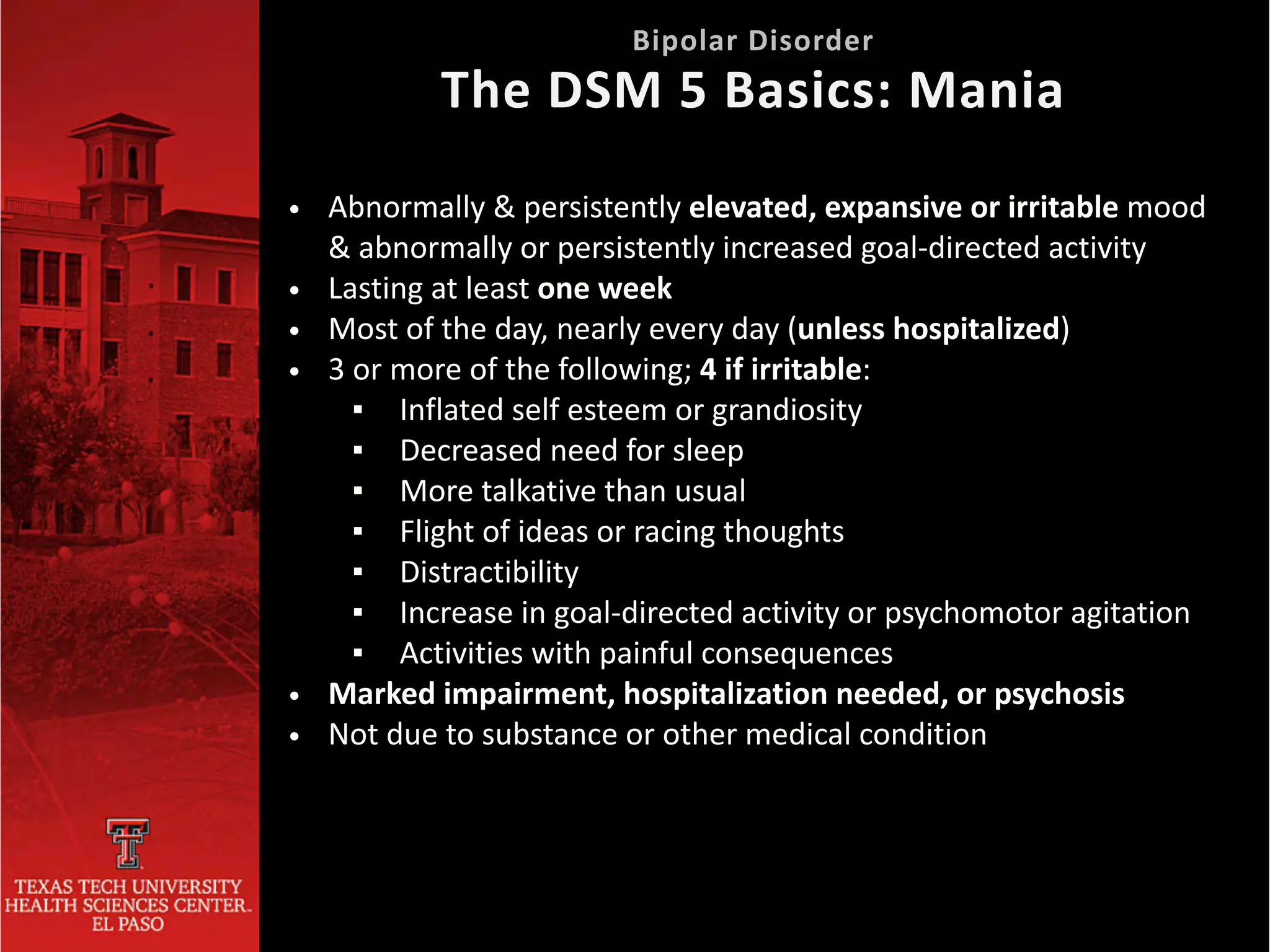
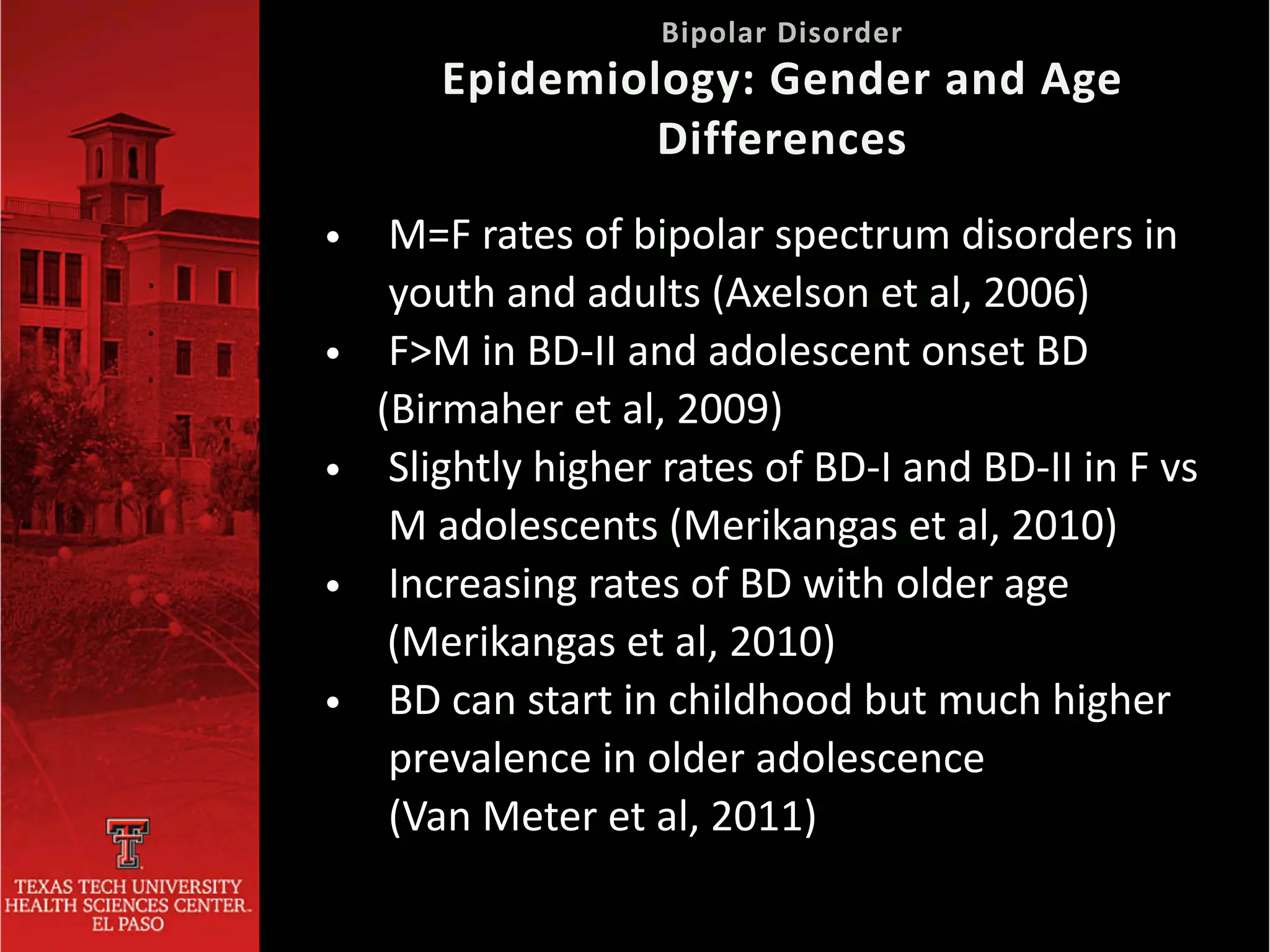
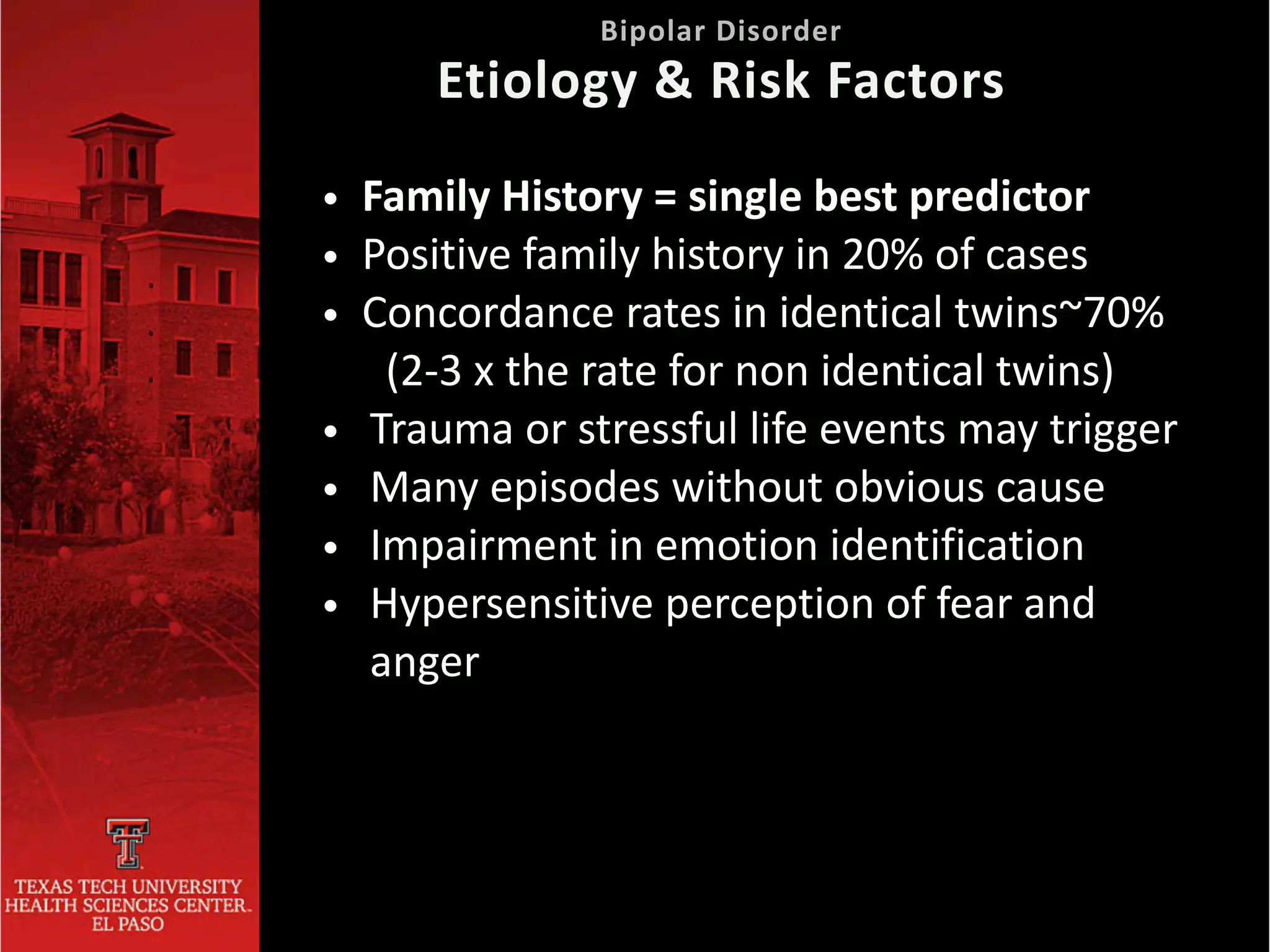
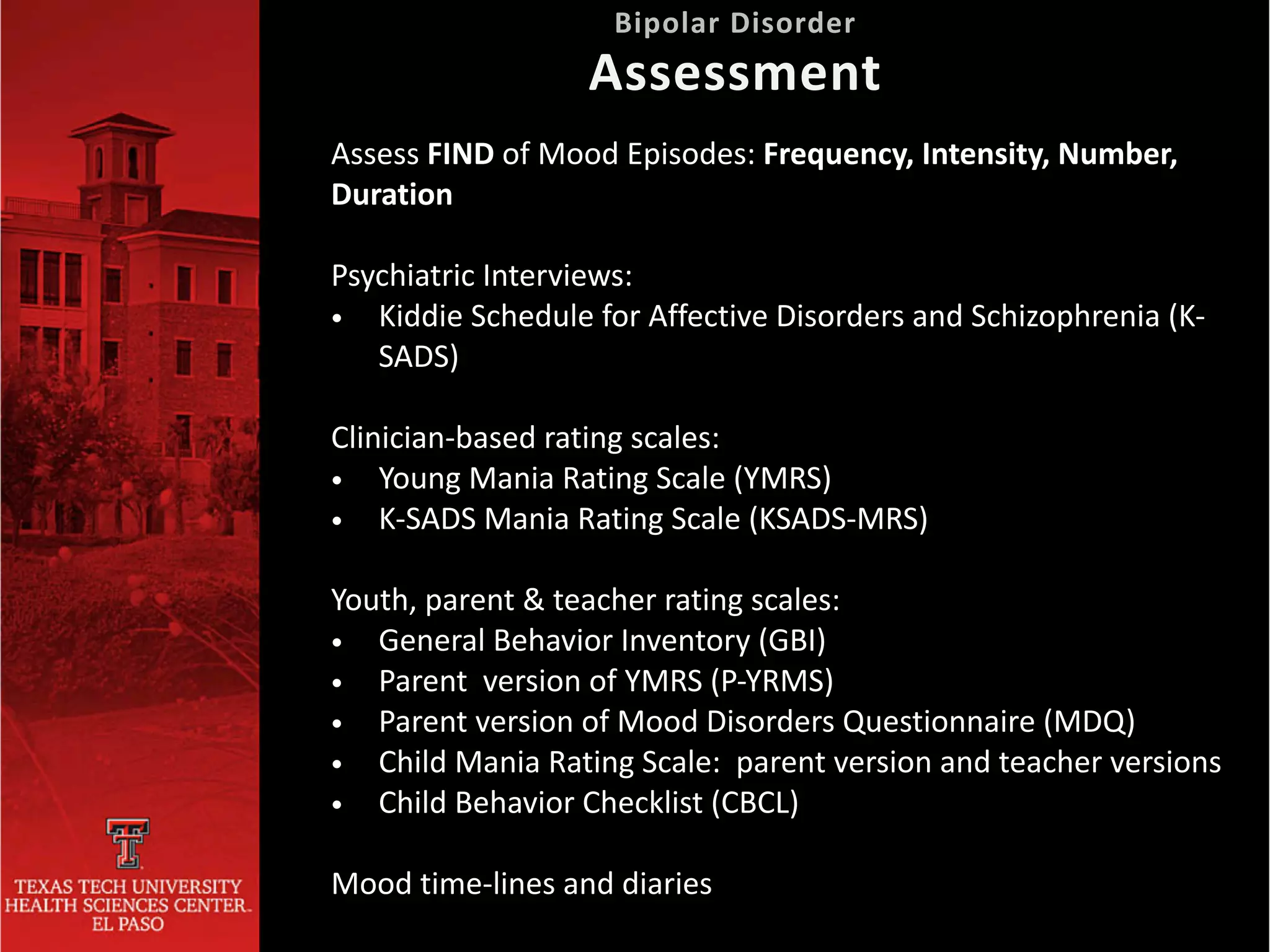
This document provides information on bipolar disorder, including its subtypes, diagnostic criteria, epidemiology, clinical presentation, etiology and risk factors, comorbidity, and treatment. It discusses bipolar disorder types I and II, as well as cyclothymic disorder. It outlines the DSM-5 diagnostic criteria for mania, hypomania, and depression. It notes the prevalence of bipolar disorder in adults and youth, gender and age of onset differences, burden of illness, and course of the disorder. It covers etiology, risk factors, and high rates of comorbidity with other psychiatric disorders. It also discusses clinical presentations, differential diagnosis, assessment, and treatment approaches including pharmacotherapy, sleep hygiene, psychosocial