- 34 year old male from Pakistan presents with fever, rigors, and sweats for 3 days after travel to Croatia 14 days prior. Physical exam is notable for fever of 102.7F but otherwise unremarkable.
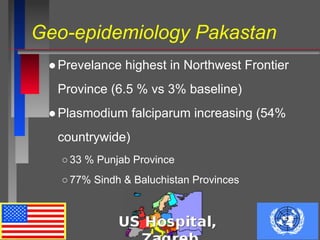
- Malaria is endemic in parts of Pakistan, transmitted by several mosquito species. P. falciparum is increasing and causes the most severe disease.
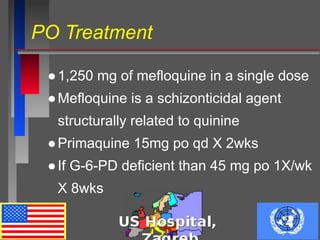
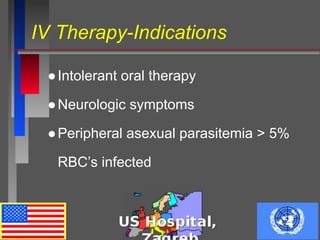
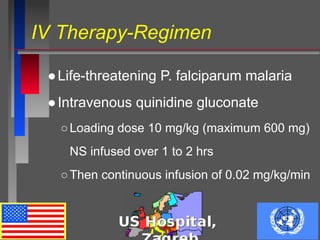
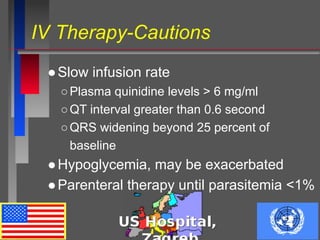
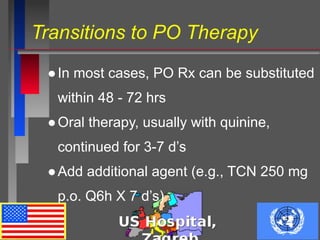
- The patient likely has malaria acquired in Pakistan or Croatia, with P. falciparum or P. vivax being the most common causes. He will be treated with intravenous quinidine followed by oral therapy if parasites decrease sufficiently.