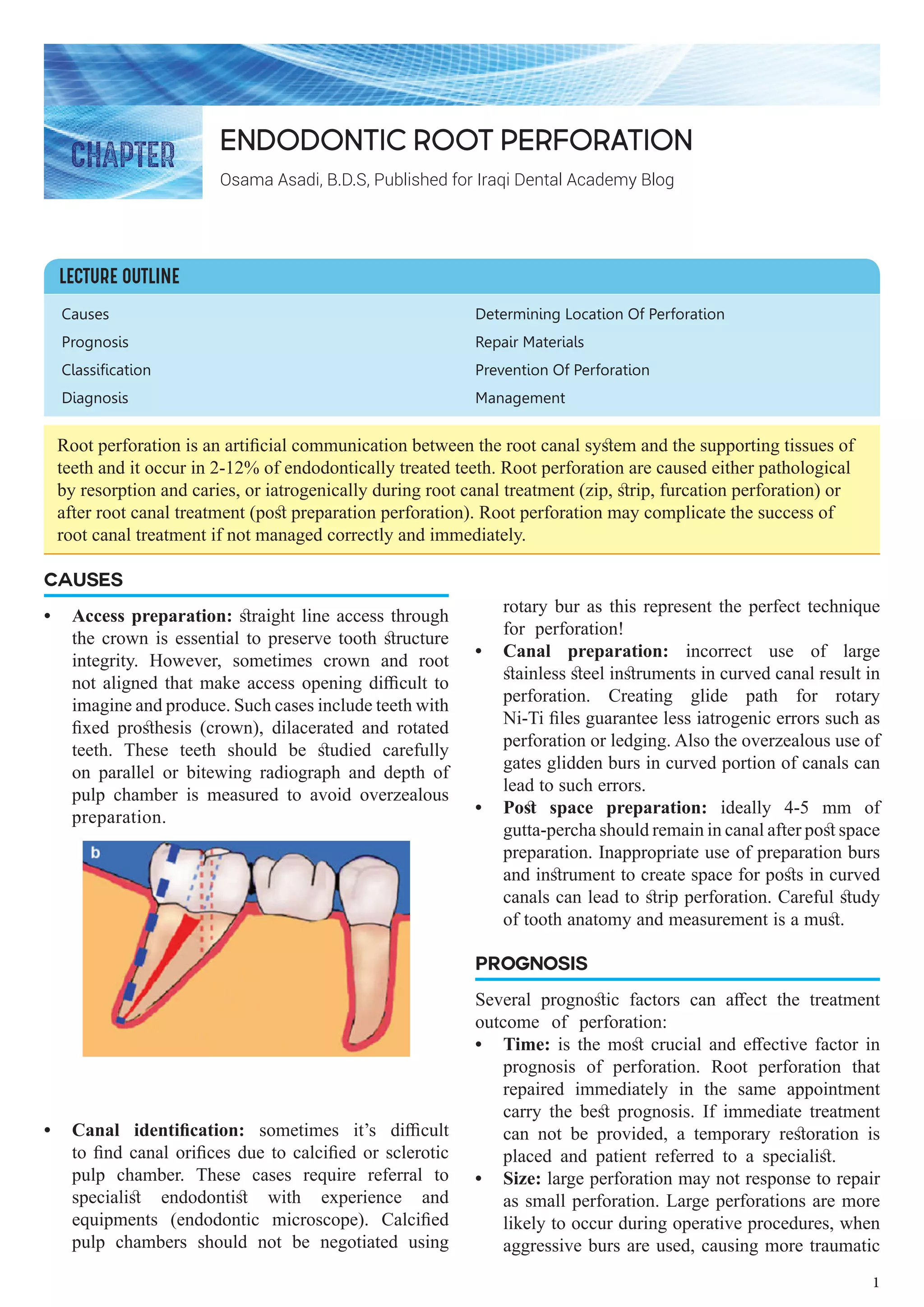
The document provides an overview of root perforation in endodontic treatment, including its causes, diagnosis, prognostic factors, management, and prevention strategies. It emphasizes the importance of immediate treatment for perforations, as delays can lead to poor prognosis, and discusses various repair materials and techniques based on the location and size of the perforation. The document also outlines the classifications of perforations and related treatment approaches, highlighting the need for careful evaluation during dental procedures to prevent such complications.