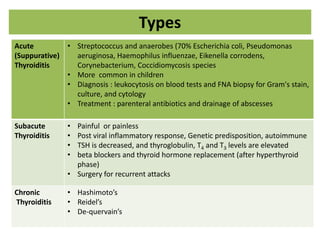
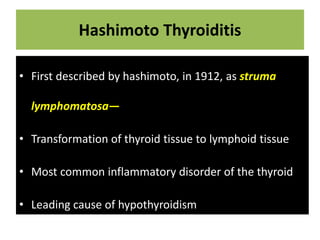
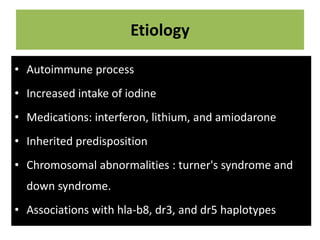
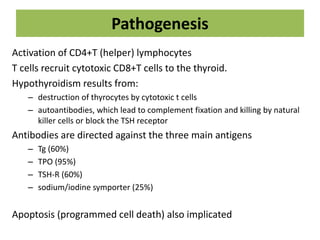
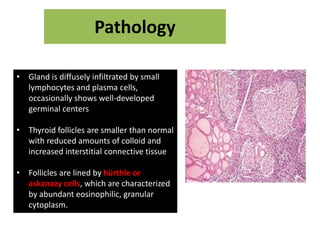
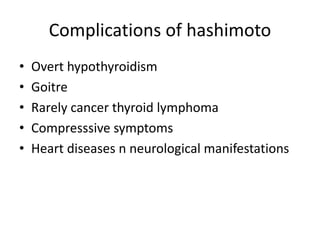
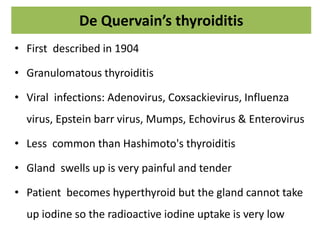
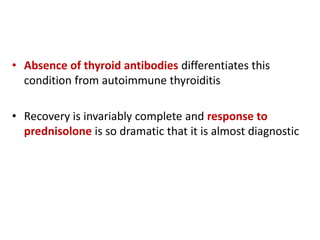
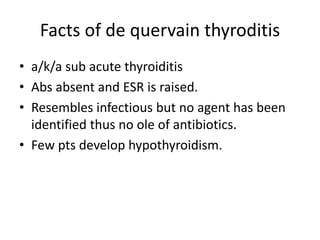
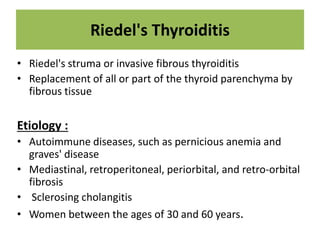
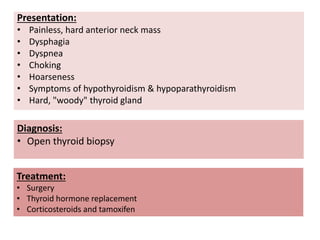
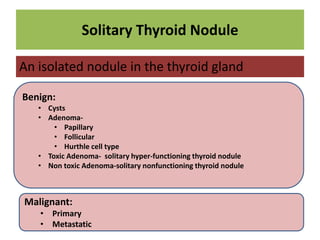
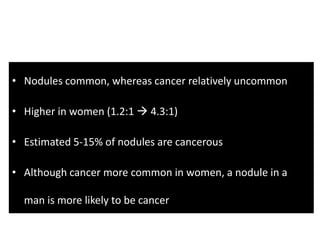
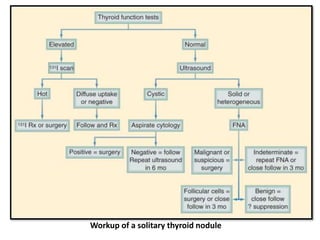
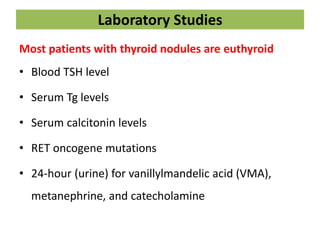
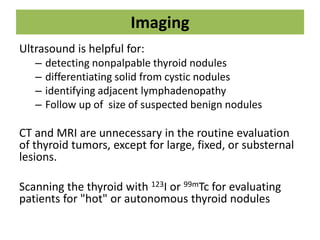
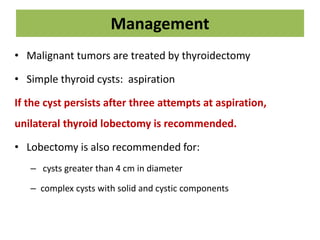
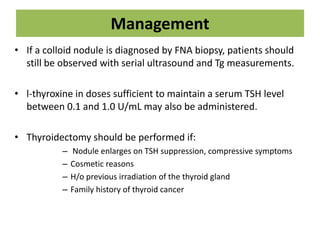
The document discusses various types of thyroiditis, including Hashimoto's, De Quervain's, and Riedel's, highlighting their pathology, etiology, clinical presentation, diagnosis, and treatment options. It emphasizes Hashimoto's thyroiditis as the most common inflammatory disorder leading to hypothyroidism, while detailing the characteristics of acute, subacute, and chronic thyroiditis. Additionally, the document provides information on solitary thyroid nodules, their benign and malignant forms, diagnostic workups, and management strategies.