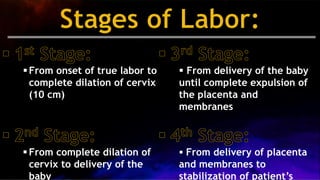
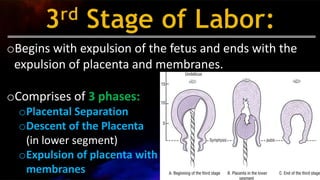
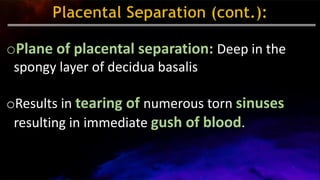
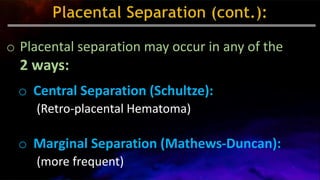
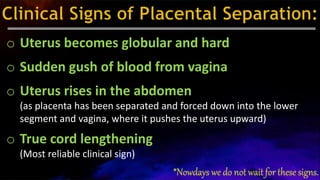
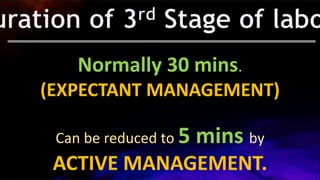
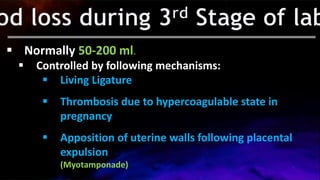
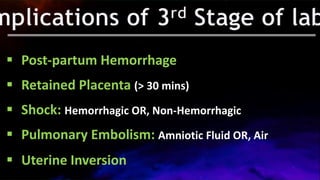
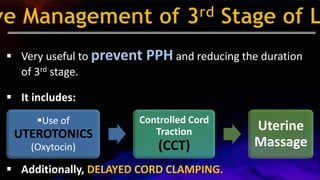
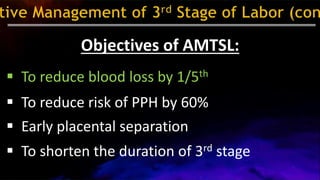
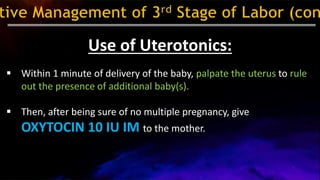
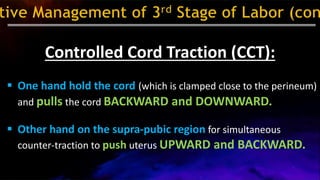
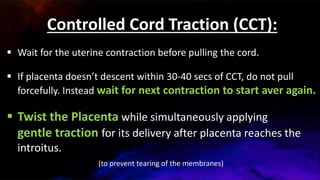
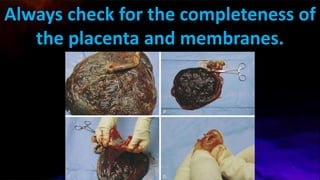
The document describes the series of events in the third stage of labor, highlighting the processes involved in expelling the placenta and membranes after childbirth. It details two management approaches: active and expectant management, with active management including the use of uterotonics and controlled cord traction to reduce postpartum hemorrhage. The document also discusses complications, signs of placental separation, and techniques for ensuring the complete expulsion of the placenta.