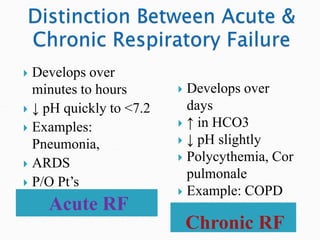
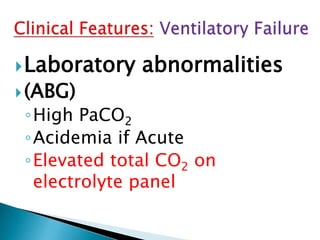
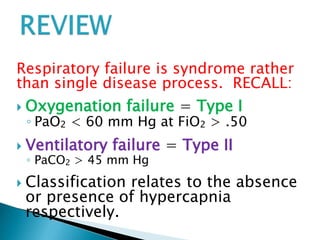
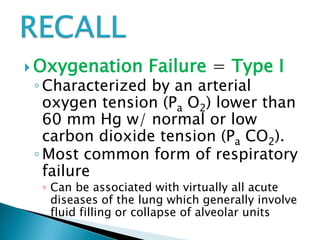
1) Respiratory failure can be caused by oxygenation failure (type I) or ventilatory failure (type II), classified based on blood gas levels of PaO2 and PaCO2.
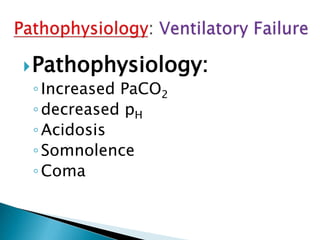
2) Oxygenation failure is characterized by low PaO2 while ventilatory failure is characterized by high PaCO2. Both can cause acidosis.
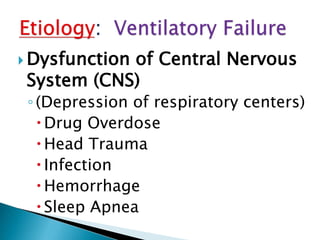
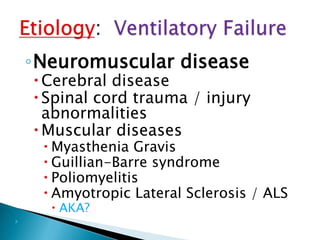
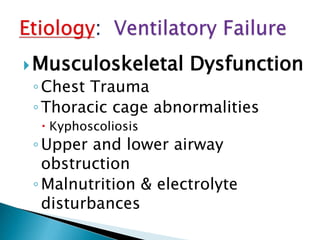
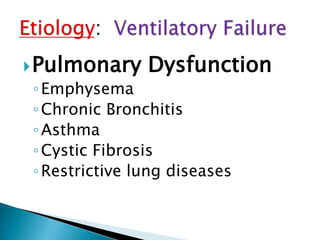
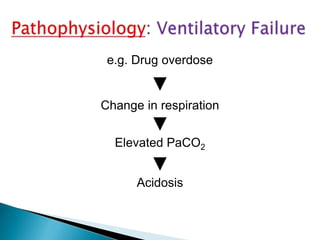
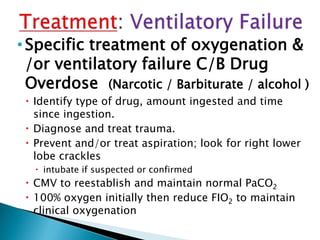
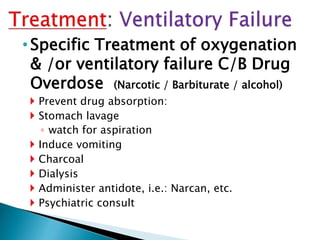
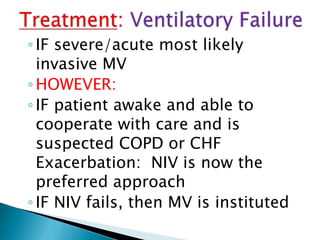
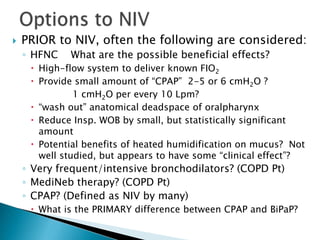
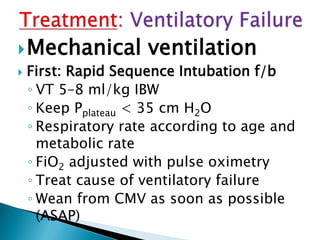
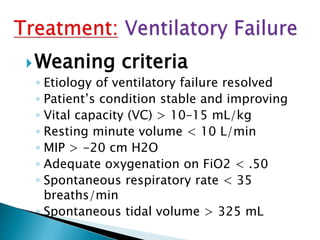
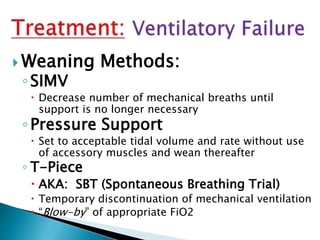
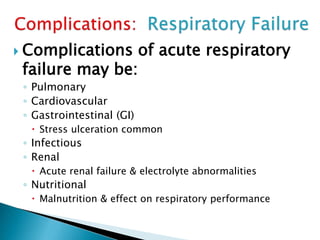
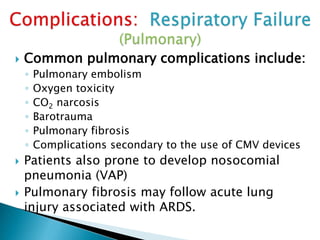
3) Causes of respiratory failure include central nervous system issues, neuromuscular diseases, pulmonary diseases like COPD, and drug overdoses. Treatment depends on the underlying cause and may include oxygen therapy, non-invasive ventilation, or mechanical ventilation.
![ Acute: abnormal elevation of the
PaCO2 without renal compensation
Chronic: abnormal elevation of the
PaCO2 with renal compensation
(abnormal Base Excess [BE] with the
pH in normal range)
Mixed: a combination of acute and
chronic (abnormal BE but the pH is not
in the normal range)](https://image.slidesharecdn.com/resp-210721000620/85/Resp-failure-type-2-ventilatory-failure-6-320.jpg)