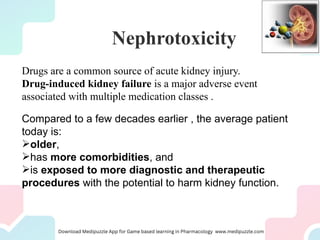
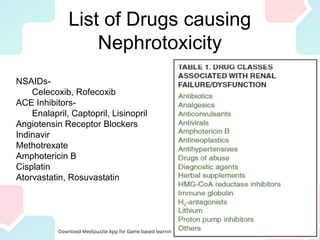
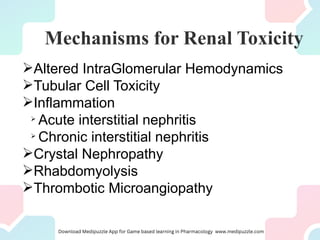
Nephrotoxic drugs can damage the kidneys by several mechanisms. Certain patient characteristics like older age, pre-existing kidney disease, and volume depletion increase risk. Common nephrotoxic drug classes include antibiotics, chemotherapy drugs, antivirals, NSAIDs, and statins. Drugs may cause acute kidney injury through effects on hemodynamics, tubular toxicity, inflammation, crystal formation, or rhabdomyolysis. Early recognition of rising creatinine and discontinuing the offending drug is important to reverse damage. Preventing nephrotoxicity requires assessing risks, monitoring for injury, and avoiding unnecessary nephrotoxic medications.