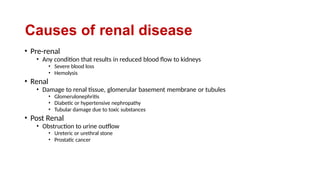
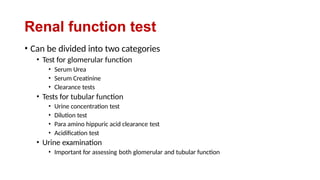
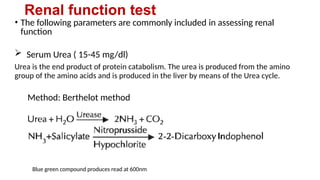
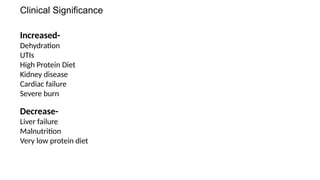
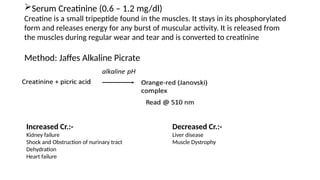
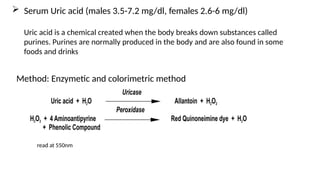
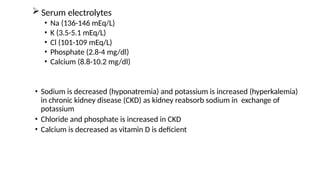
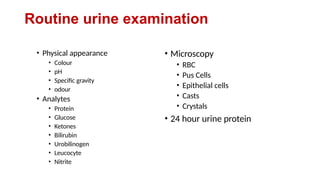
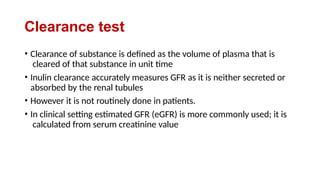
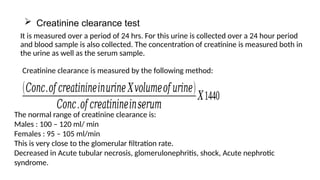
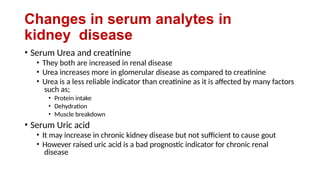
The document outlines renal function tests, their objectives, and the various kidney functions including excretory, homeostatic, endocrine, and metabolic roles. It specifies common biochemical tests for assessing kidney function, including serum urea, creatinine, and urine examination, highlighting their significance and changes in levels associated with renal impairment. Additionally, it discusses causes of renal disease categorized as pre-renal, renal, and post-renal, along with testing methods for glomerular and tubular functions.