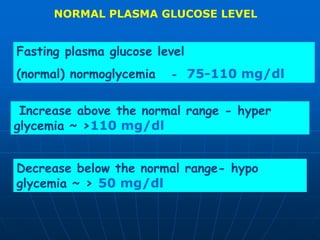
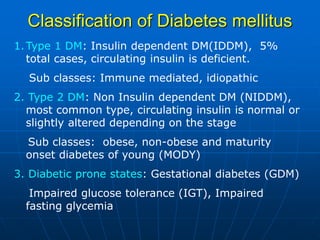
The document discusses regulation of blood glucose levels and metabolic derangements in diabetes. It describes how hormones like insulin and glucagon tightly regulate blood glucose levels by controlling glucose uptake and release. In diabetes, there is either insufficient insulin production or insulin resistance, leading to hyperglycemia. This causes symptoms like excessive thirst and urination as the body tries to eliminate excess glucose through urine. Without treatment, high blood glucose in diabetes can cause serious complications like diabetic ketoacidosis or hyperosmolar coma.