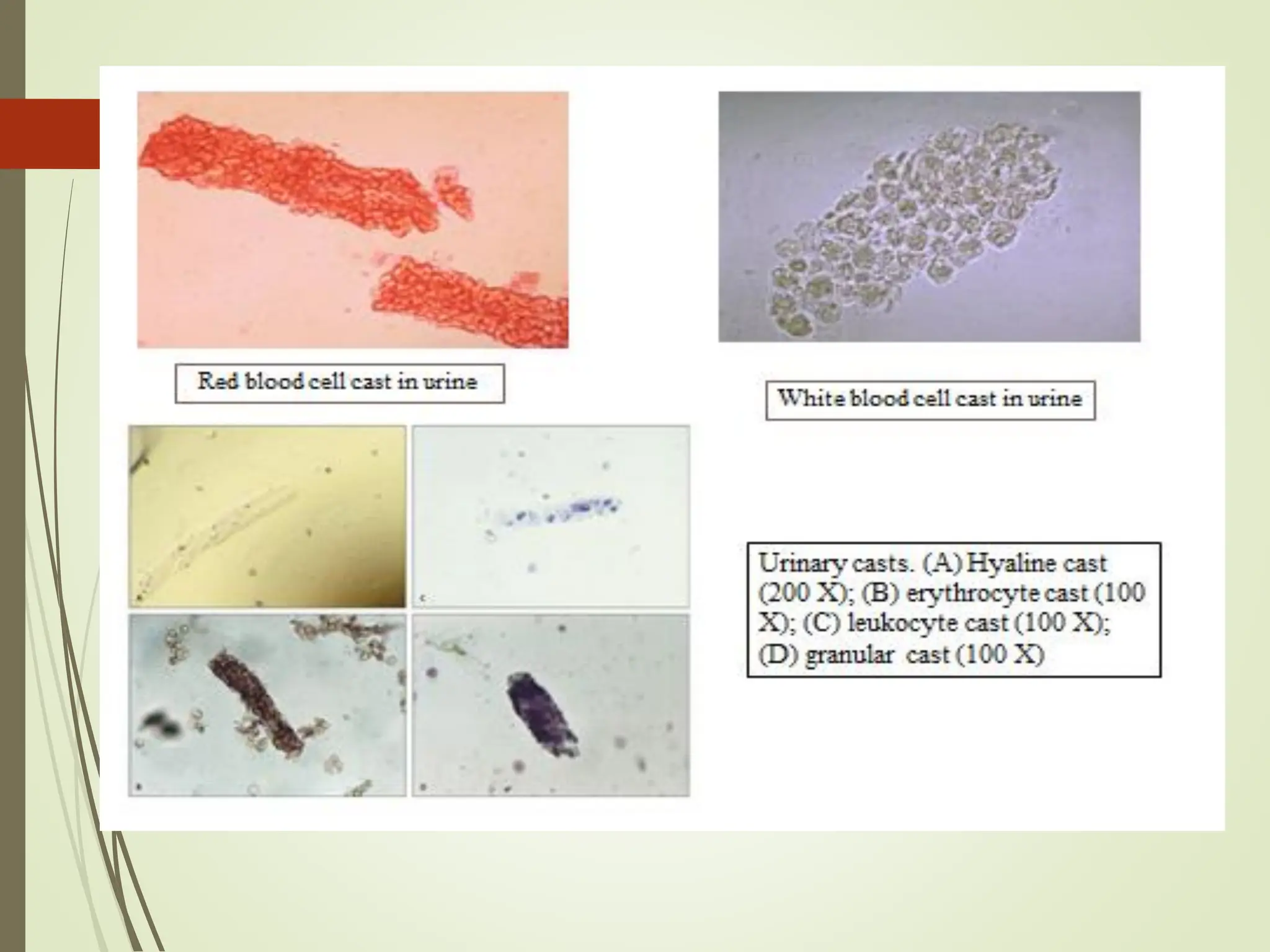
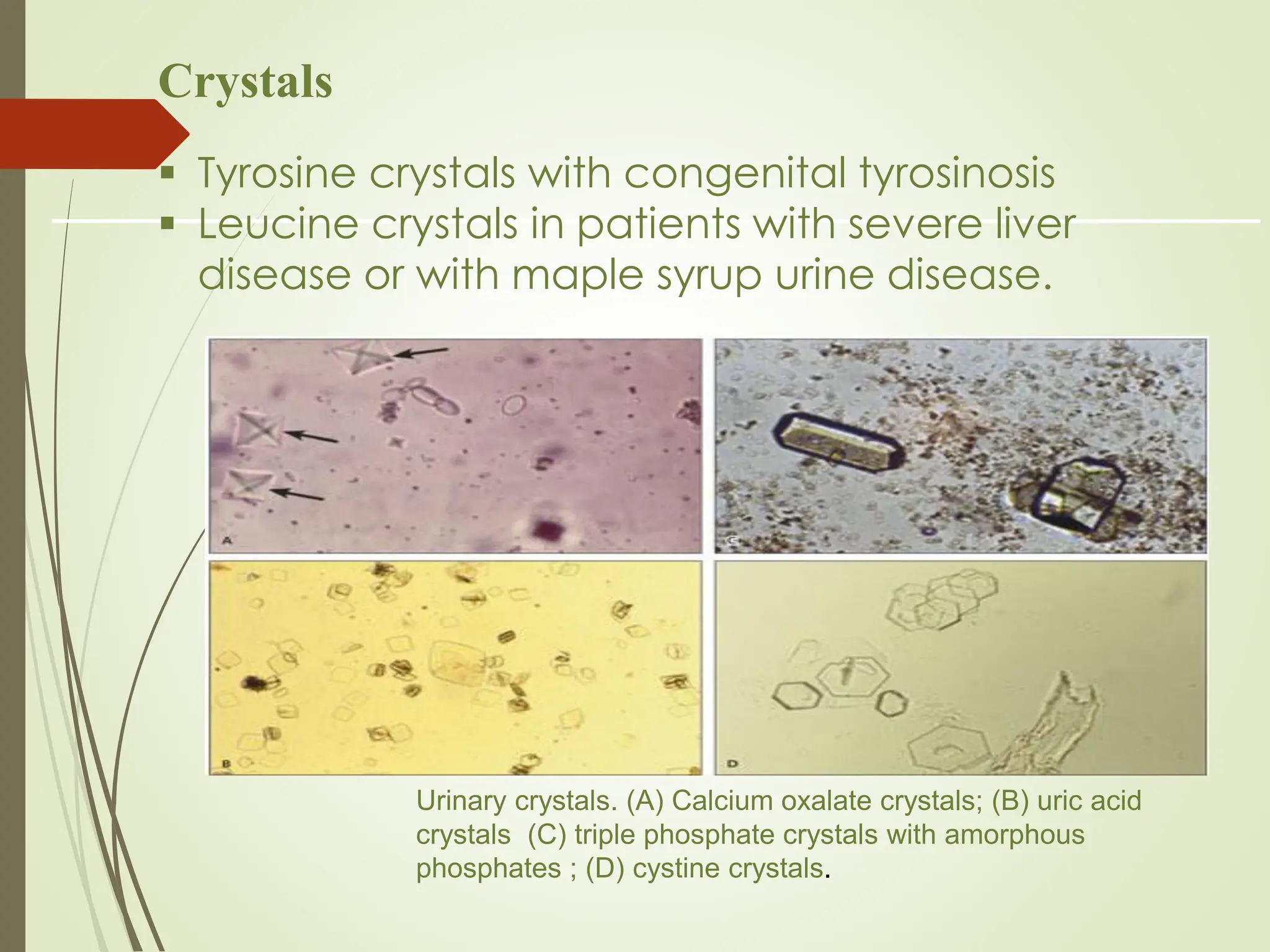
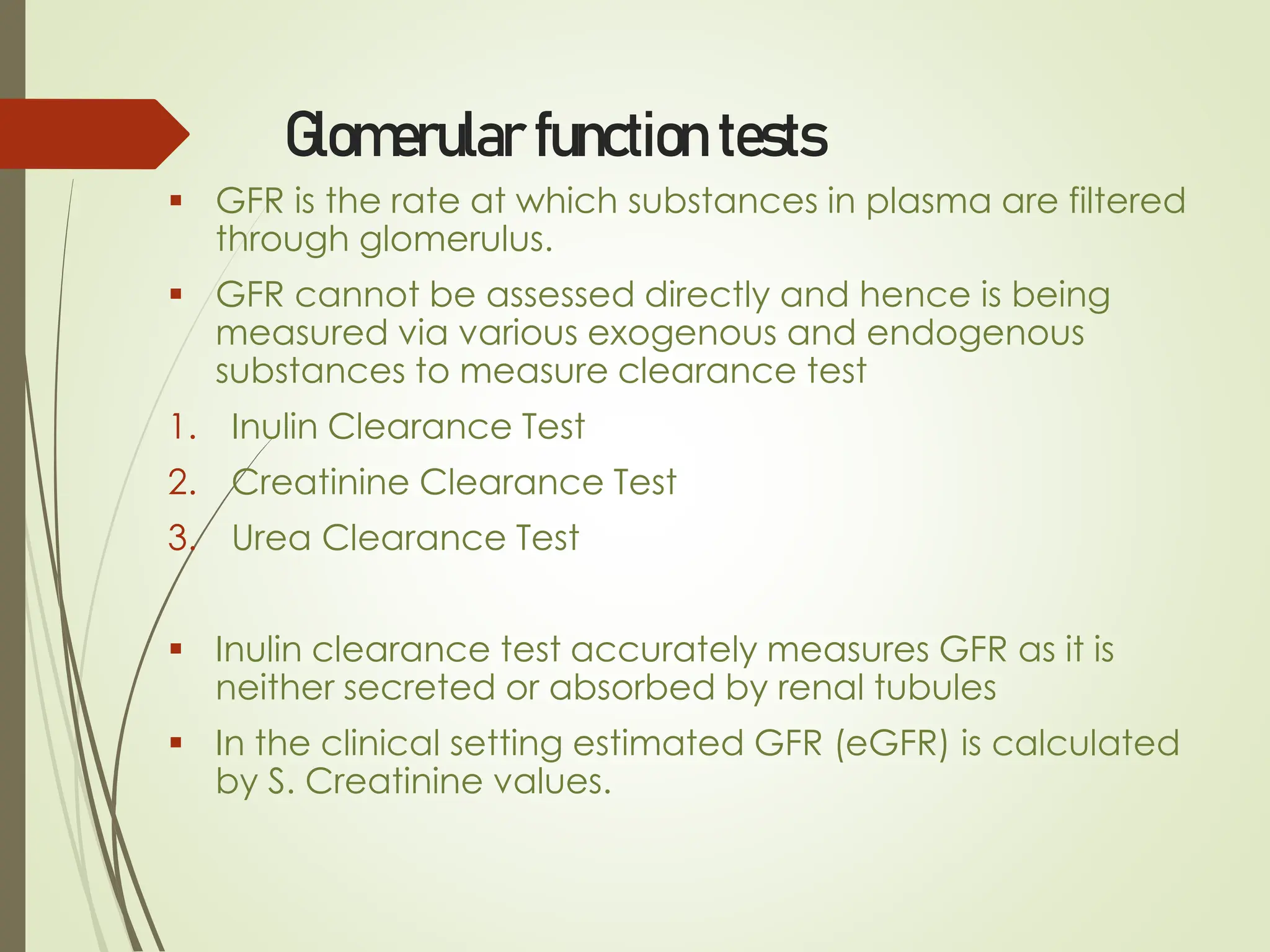
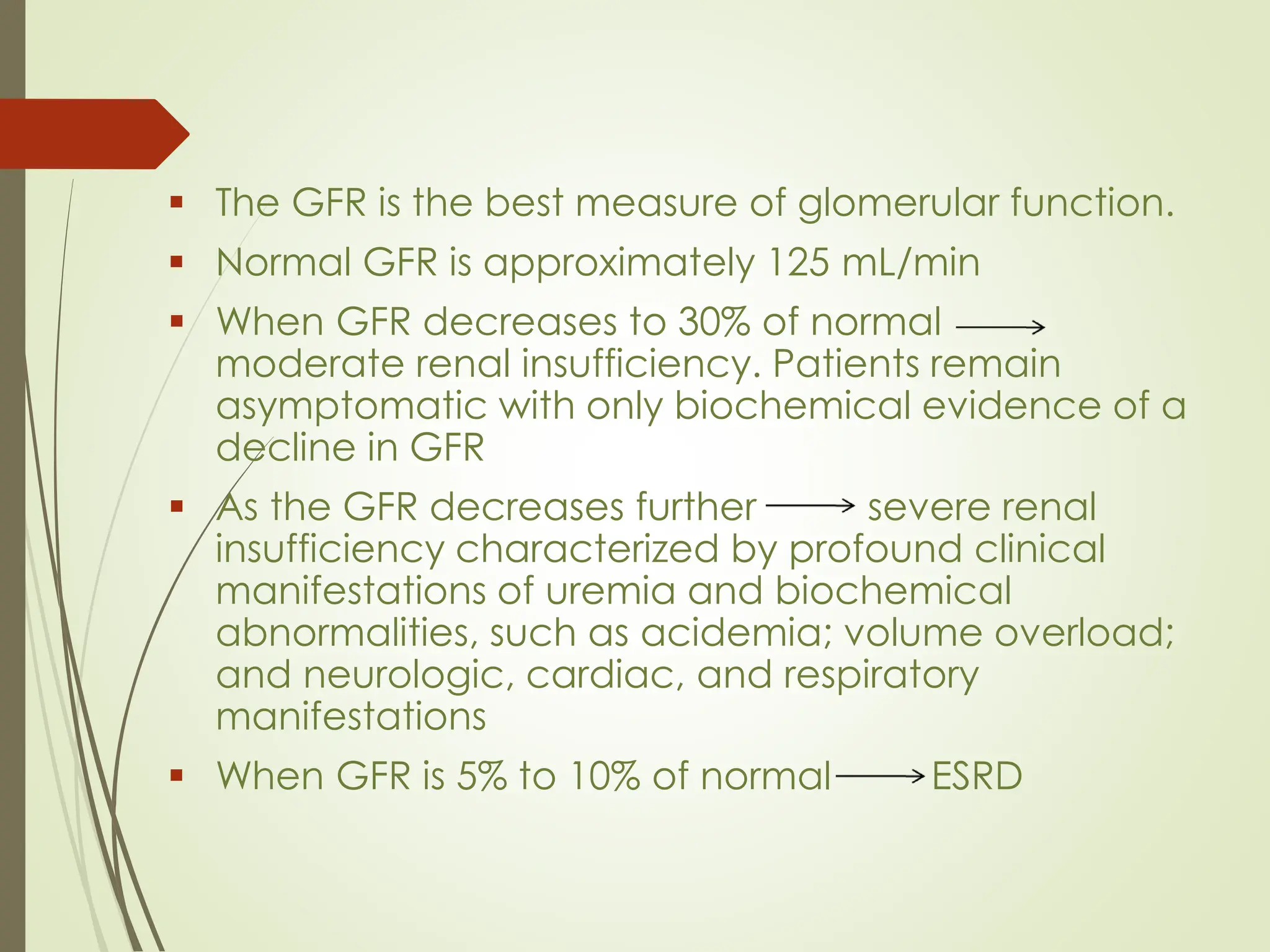
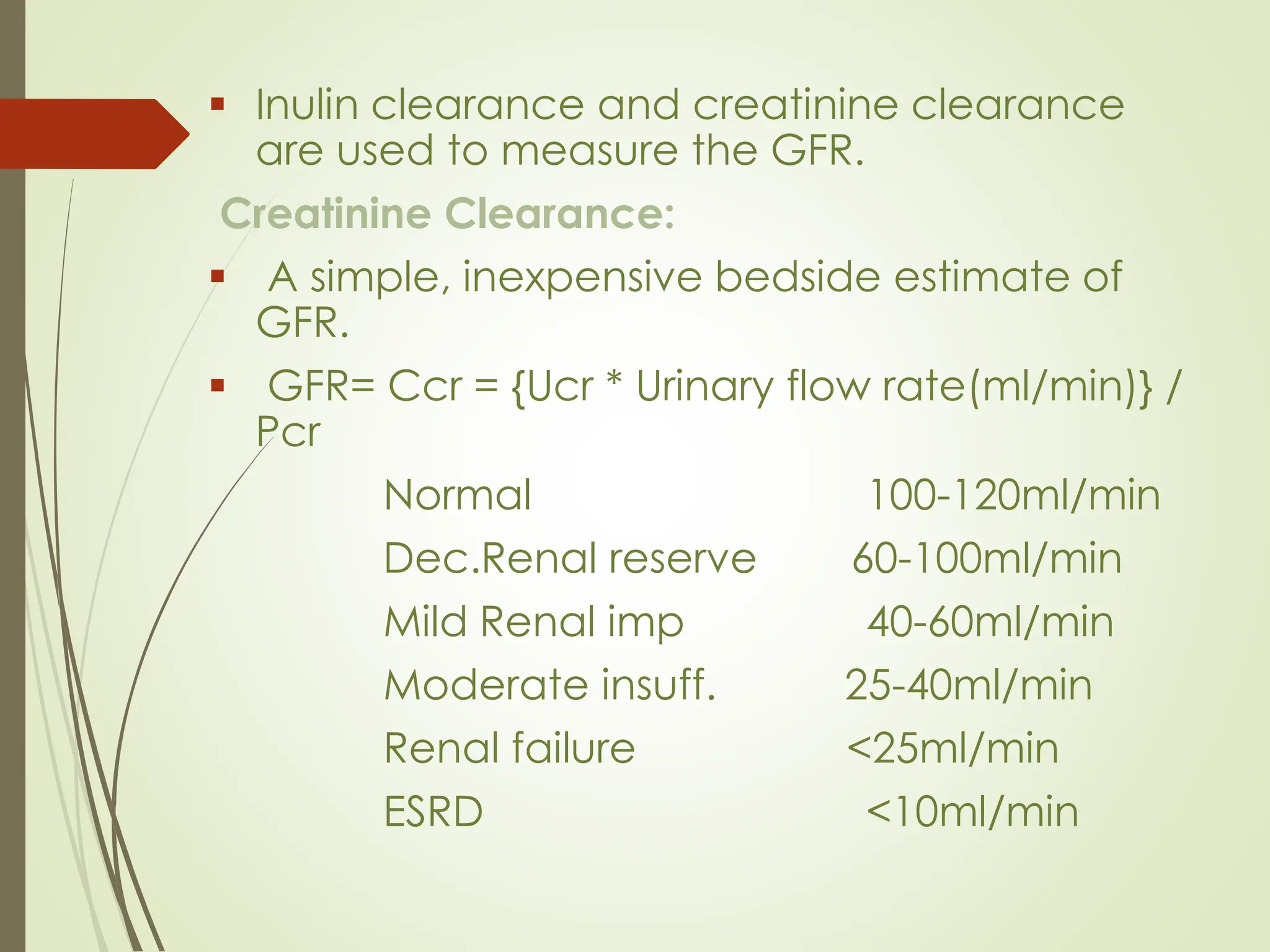
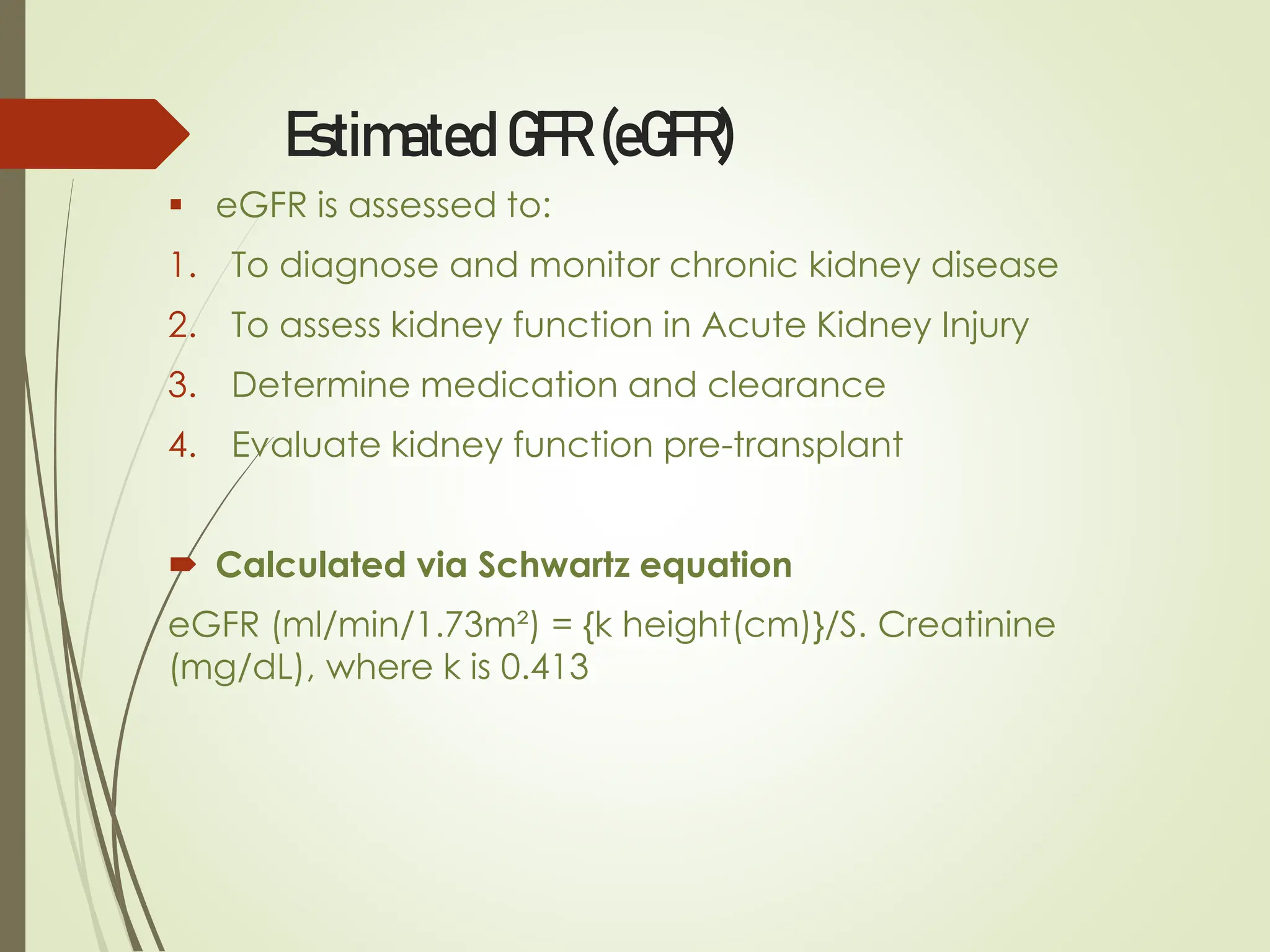
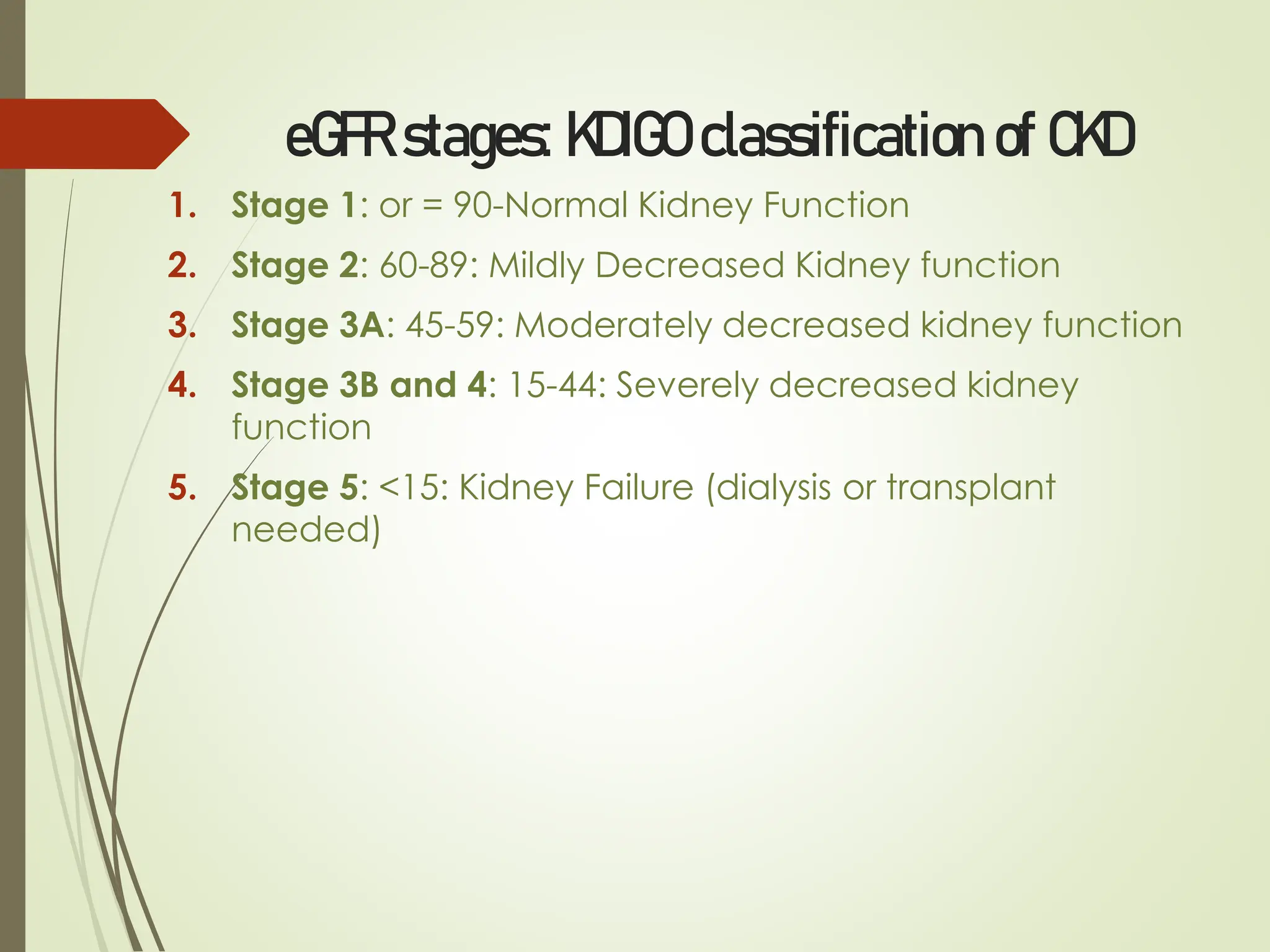
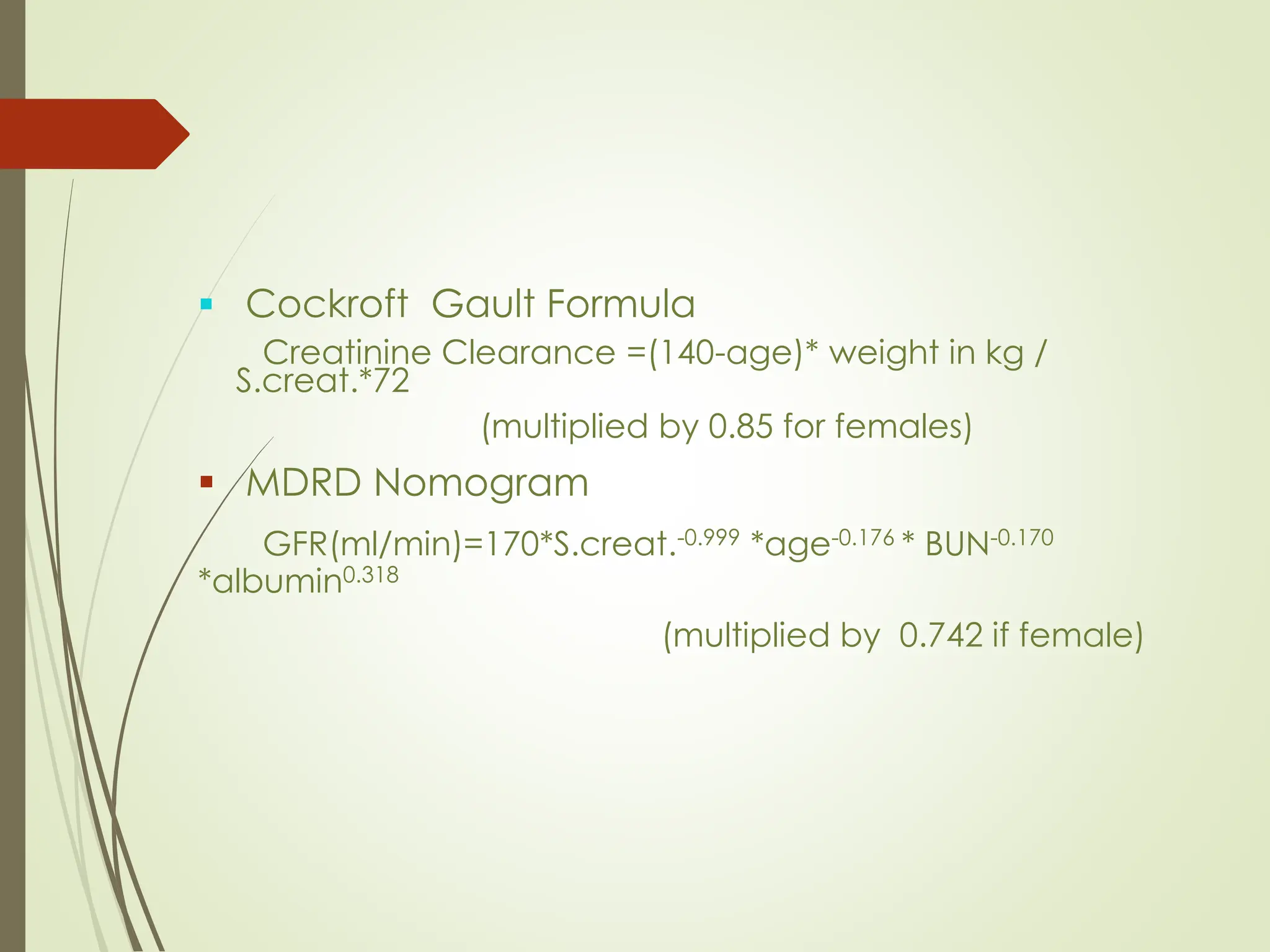
The document provides a comprehensive overview of renal function tests, which assess kidney performance, including regulation of ions, water balance, and waste excretion. It covers the purpose of these tests, indications for assessment, common symptoms of renal impairment, and classification of tests such as urine analysis and blood examination. Additionally, it discusses various tests for glomerular and tubular function, emphasizing the importance of monitoring kidney function to detect and manage renal diseases effectively.