This document provides a comprehensive overview of kidney function tests (KFTs) and their significance in assessing renal health. It details the anatomy of the nephron, the functions of kidneys, and the parameters involved in KFTs, including urine examination, serum creatinine, and blood urea nitrogen levels. It also discusses the interpretation of results and the implications of various conditions linked to renal impairment.
![1
SOME BASIC CONCEPTS OF BIOCHEMISTRY FOR DMLT SECOND YEAR STUDENTS (U.
P. State Medical Faculty syllabus) in Hinglish
LESSON 8
[Kidney function tests (KFT)/Renal function tests (RFT)/Renal panel]
IN ENGLISH
KIDNEY FUNCTION TESTS
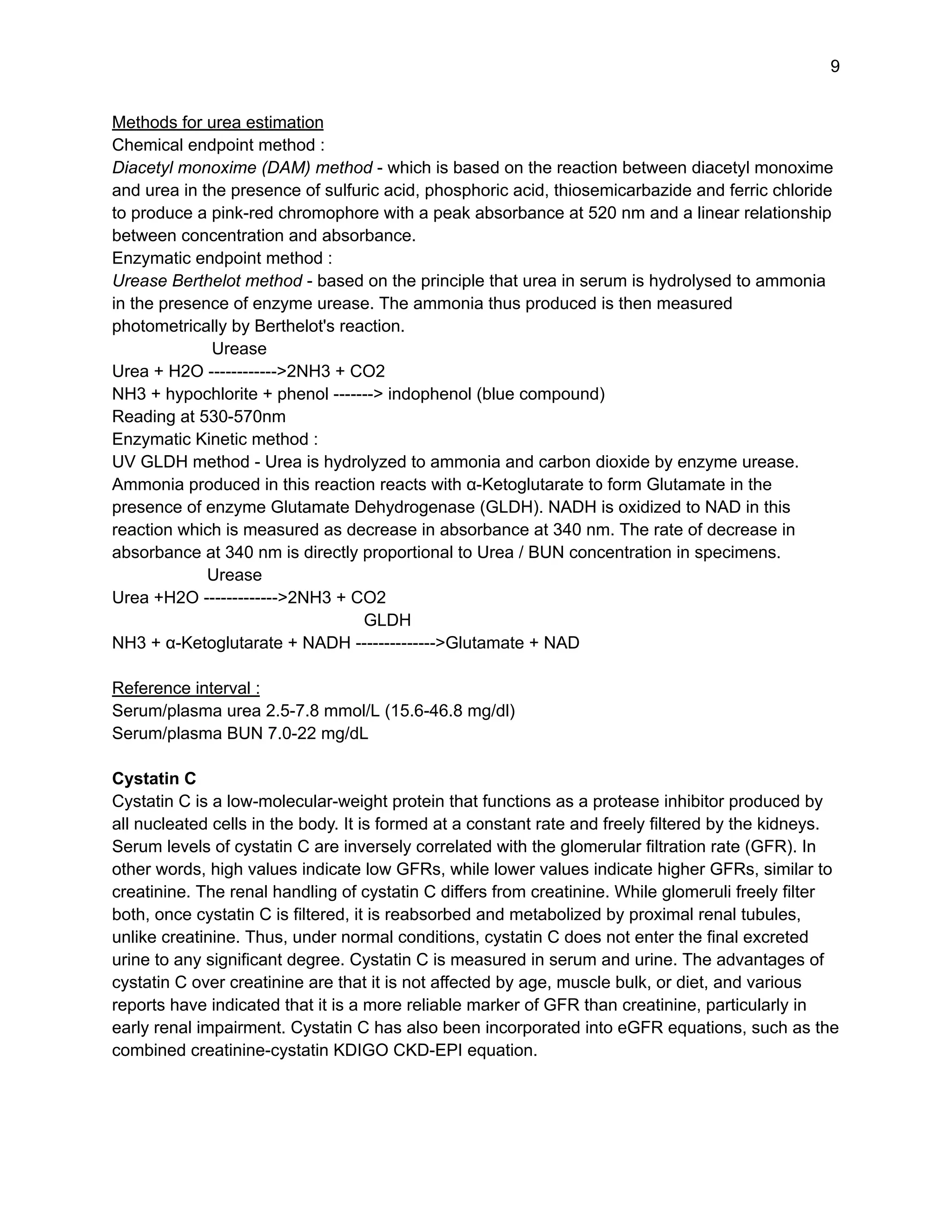
Nephron
The functional units of the kidney are the nephron, which consists of the glomerulus, proximal
and distal tubules, and collecting duct.
Functions of kidneys
● Excretion of waste products and toxins such as urea, creatinine and uric acid,
● Regulation of extracellular fluid volume, serum osmolality and electrolyte concentrations,
● Production of hormones like erythropoietin and 1,25 dihydroxy vitamin D and renin.
Assessment of renal function is important in :
● the management of patients with kidney disease or pathologies affecting renal function.
● identifying the presence of renal disease,
● monitoring the response of kidneys to treatment, and
● determining the progression of renal disease.
Parameters of renal function tests
● Urine - routine and microscopic examination
● Glomerular Filtration Rate
● Serum creatinine
● Serum urea or blood urea nitrogen (BUN)
● Serum cystatin C](https://image.slidesharecdn.com/dmlt2kft-241225081037-2c451038/75/DMLT-2nd-Year-Kidney-Function-Tests-Some-basic-concepts-U-P-State-Medical-Faculty-syllabus-in-English-Hinglish-1-2048.jpg)
![2
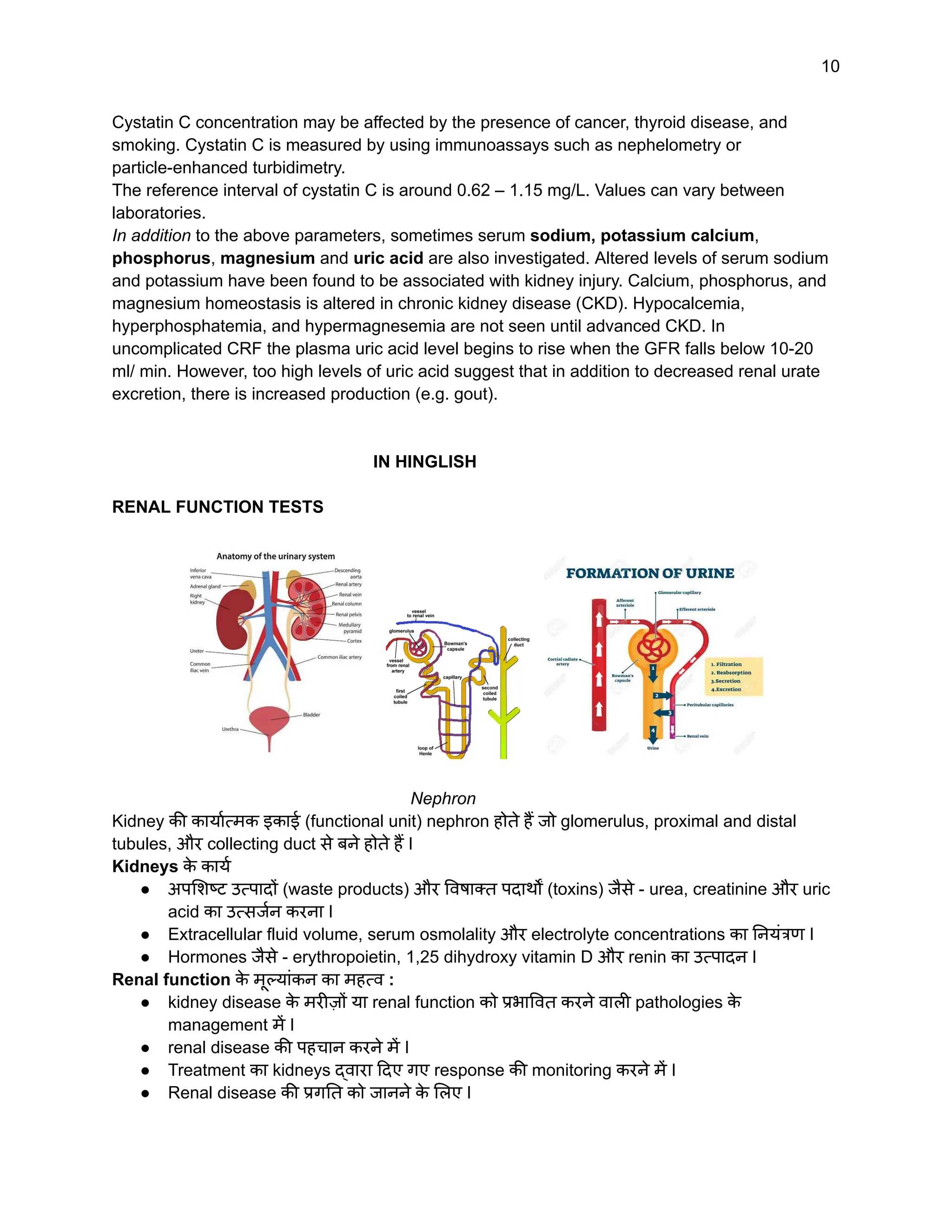
Urine examination
Routine examination
Appearance - Indication
Straw coloured - normal
Dark in colour - dehydration
Red colour - hematuria or porphyria or could be due to dietary intake of
food like beets.
Clear - normal
Cloudy - pyuria (urinary tract infection, UTI)
Specific gravity (an indicator of the renal concentrating ability)
1.003 to 1.030 - normal
Increased (>1.030) - low water intake/diabetes mellitus/albuminuria/acute
nephritis
pH
6.0-6.5 (acidic) - normal
High (alkaline) - kidney stones/UTIs/ kidney-related disorders
Low (more acidic) - diabetic ketoacidosis/diarrhea/ starvation
Chemical examination
Dipstick uses dry chemistry methods to detect the presence of protein, glucose, blood, ketones,
bilirubin, urobilinogen, nitrite, and leukocyte esterase. However, the analyte of interest in renal
function tests is - protein. Normal urine protein is up to 150 mg per day [30% albumin; 30%
globulins; 40% Tamm Horsfall protein (Uromodulin, a glycoprotein)] and its rising levels indicate
a kidney problem. Albuminuria refers to the abnormal presence of albumin in the urine.
Sometimes a term microalbuminuria is used but now it is considered an obsolete term as there
is no such biochemical molecule, and hence it is referred to only as urine albumin.
● Albuminuria is used as a marker for the detection of incipient nephropathy (the initial
presence of low but abnormal amounts of urine albumin) in diabetics.
● It is an independent marker for the cardiovascular disease since it suggests increased
endothelial permeability.
● It is also a marker for chronic renal impairment.
For testing albuminuria the urine may be collected normally in three ways:
● In a special container (with preservative) over a 24-hour period for urinary albumin
excretion (UAE) determination.
● A urine sample first thing in the morning or after a four-hour period of not urinating
(Timed urine test) for albumin excretion rate (AER) determination.
● A random (spot) urine sample can be taken at any time for urinary albumin concentration
(UAC) estimatiion but to improve the accuracy of the results, it's often combined with a
urine test for creatinine for albumin : creatinine ratio (ACR).
Estimation of albumin - can be done by immunoturbidimetric assay and HPLC.
Calculations -
Albumin (mg/dl)
ACR (mg/g) = ------------------------ x 1000.
Creatinine (mg/dl)](https://image.slidesharecdn.com/dmlt2kft-241225081037-2c451038/75/DMLT-2nd-Year-Kidney-Function-Tests-Some-basic-concepts-U-P-State-Medical-Faculty-syllabus-in-English-Hinglish-2-2048.jpg)
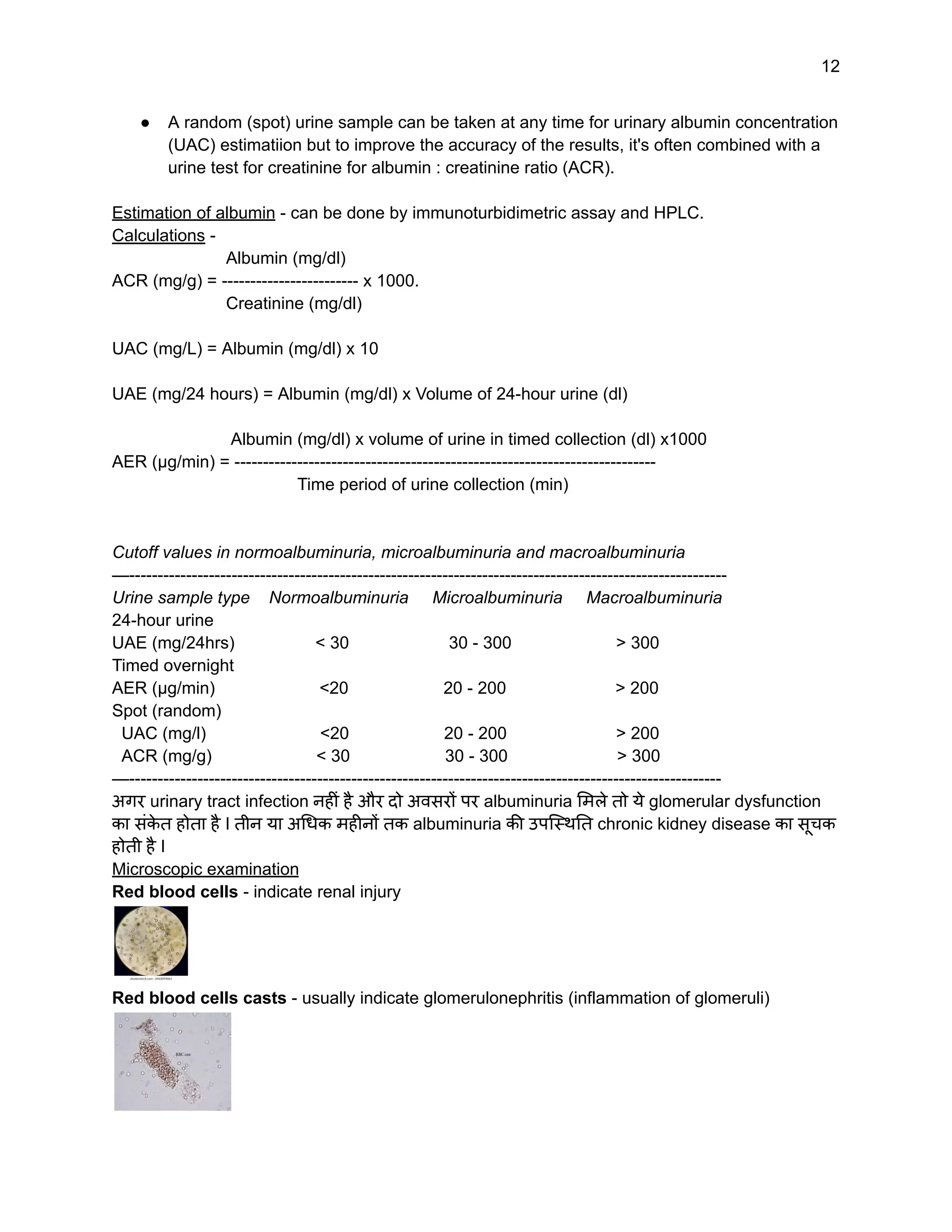
![5
Cystine crystals - are observed in cystinuria
Glomerular Filtration Rate (GFR) - is the best overall indicator of the glomerular function. GFR
is the rate in milliliters per minute at which substances in plasma are filtered through the
glomerulus. The normal GFR for an adult is 90 to 120 mL per minute.
Exogenous markers of GFR -
● Inulin clearance - It involves the infusion of inulin (a small polysaccharide) and then the
measurement of blood levels of inulin after a specified period to determine the rate of
clearance of inulin. This is the 'reference method' for determining GFR.
● Other exogenous markers used are non-radioactive contrast agent, iohexol and
radioisotopes such as chromium-51 ethylene-diamine-tetra-acetic acid (51 Cr-EDTA),
and technetium-99-labeled diethylene-triamine-pentaacetate (99 Tc-DTPA).
Due to inconvenience involved and requirement of specialized centres for performing these
tests, the use of endogenous markers of GFR is encouraged.
Endogenous markers of GFR
Plasma/serum Creatinine and urinary creatinine - is the most commonly used endogenous
marker for the assessment of glomerular function. Urinary creatinine involves the collection of
urine over a 24-hour period or preferably over an accurately timed period of 5 to 8 hours since
24-hour collections are notoriously unreliable. Creatinine clearance is then calculated using the
equation:
C = (U x V) / P
C = clearance, U = urinary creatinine concentration(mg/L) V = urinary flow rate (volume/time i.e.
ml/min), and P = plasma creatinine concentration(mg/L)
The creatinine clearance test is a method of assessing estimated GFR (eGFR).
[Important - Twenty-four-hour urine collection bottles may contain small amounts of
preservatives such as boric acid, hydrochloric acid, acetic acid, oxalic acid and thymol, and
therefore, the patient should be told that the direct contact with skin and mucous membranes
must be avoided]
The creatinine clearance test is not used very often any more. It has largely been
replaced by the eGFR equations using serum creatinine (SCr) levels.](https://image.slidesharecdn.com/dmlt2kft-241225081037-2c451038/75/DMLT-2nd-Year-Kidney-Function-Tests-Some-basic-concepts-U-P-State-Medical-Faculty-syllabus-in-English-Hinglish-5-2048.jpg)
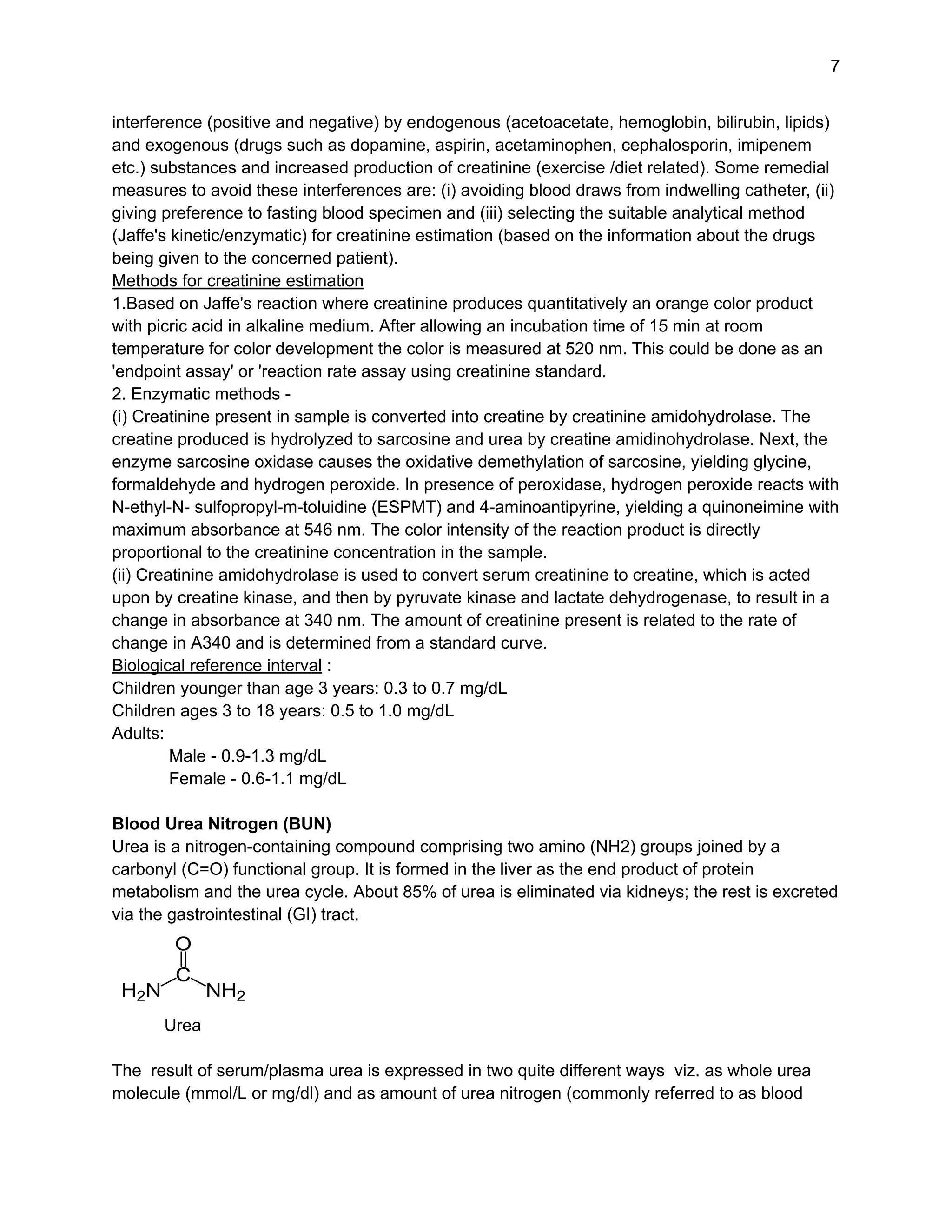
![6
In adults, the most widely-used equations for estimating glomerular filtration rate (GFR) from
serum creatinine are the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI)
equation and the isotope dilution mass spectrometry (IDMS) traceable Modification of Diet in
Renal Disease (MDRD) Study equation.
The CKD-EPI equation
GFR = 141 × min(Scr/κ, 1)α × max(Scr/κ, 1)-1.209 × 0.993Age × 1.018 [if female] × 1.159 [if
African American]
where:
Scr is serum creatinine in mg/dL,
κ is 0.7 for females and 0.9 for males,
α is -0.329 for females and -0.411 for males,
min indicates the minimum of Scr/κ or 1, and
max indicates the maximum of Scr/κ or 1
These eGFR equations are superior to serum creatinine alone since they include race, age, and
gender variables. eGFR equations are used to determine the presence of renal disease, stage
of CKD, and to monitor response to treatment.
—----------------------------------------------------------------------------------------------------------------------------
STAGES OF CHRONIC KIDNEY DISEASE GFR % OF KIDNEY FUNCTION
Stage 1 Kidney damage with normal kidney function 90 or high 90 - 100%
Stage 2 Kidney damage with mild loss of kidney function 89 - 60 89 - 60%
Stage 3a Mild to moderate loss of kidney function 59 - 45 59 - 60%
Stage 3b Moderate to severe loss of kidney function 44 - 30 44 - 30%
Stage 4 Severe loss of kidney function 29 - 15 29 - 15%
Stage 5 Kidney failure < 15 < 15%
—----------------------------------------------------------------------------------------------------------------------------
Serum creatinine - Creatinine is the by-product of creatine phosphate in muscle, and it is
produced at a constant rate by the body. For the most part, creatinine is cleared from the blood
entirely by the kidney. Decreased clearance by the kidney results in increased blood creatinine
and increased level of creatinine may be a sign of poor kidney function. The amount of
creatinine produced per day depends on muscle mass and diet. Additionally, serum creatinine
is a later indicator of renal impairment because renal function is decreased by 50% before a rise
in serum creatinine is observed.
Causes of increased serum creatinine
With Decreased GFR -
● Prerenal - due to shock/hemorrhage, dehydration, congestive cardiac failure.
● Renal - acute and chronic renal failure
● Post-renal - obstructive lesions of the urinary tract
Blood collection for serum creatinine estimation -
For serum creatinine test no special preparation is required by the patient but false estimates of
serum creatinine have been found due to interference by both exogenous and endogenous
substances which have been attributed to factors such as decreased or inhibited tubular
secretion of creatinine (due to drugs such as cimetidine, ranitidine, trimethoprim etc.),](https://image.slidesharecdn.com/dmlt2kft-241225081037-2c451038/75/DMLT-2nd-Year-Kidney-Function-Tests-Some-basic-concepts-U-P-State-Medical-Faculty-syllabus-in-English-Hinglish-6-2048.jpg)
![11
Renal function tests क
े मुख्य मापदण्ड (main parameters) :
● Urine - routine and microscopic examination
● Glomerular Filtration Rate
● Serum creatinine
● Serum urea or blood urea nitrogen (BUN)
● Serum cystatin C
Urine examination
Routine examination
Appearance - Indication
Straw coloured - normal
Dark in colour - dehydration
Red colour - hematuria or porphyria or could be due to dietary intake of
food like beets.
Clear - normal
Cloudy - pyuria (urinary tract infection, UTI)
Specific gravity (an indicator of the renal concentrating ability)
1.003 to 1.030 - normal
Increased - low water intake/diabetes mellitus/albuminuria/acute
nephritis
pH
6.0-6.5 (acidic) - normal
High (alkaline) - kidney stones/UTIs/ kidney-related disorders
Low (more acidic) - diabetic ketoacidosis/diarrhea/ starvation
Chemical examination
Dipstick uses dry chemistry methods to detect the presence of protein, glucose, blood, ketones,
bilirubin, urobilinogen, nitrite, and leukocyte esterase. हालांकि renal function tests क
े लिए urinary
protein में अधिक रूचि होती है I Normal urine protein is up to 150 mg per day [30% albumin; 30%
globulins; 40% Tamm Horsfall Protein (Uromodulin, a glycoprotein)] and its rising levels indicate
a kidney problem. Albuminuria urine में albumin की असामान्य उपस्थिति को संदर्भित (refer) करता है I
कभी - कभी एक शब्द microalbuminuria का भी इस्तेमाल होता है किन्तु अब यह शब्द (microalbuminuria)
अप्रचलित (obsolete) समझा जाता है क्योंकि ऐसा कोई biochemical molecule नहीं है, और इसलिए इसे
urine albumin द्वारा ही संदर्भित (refer) किया जाता है I
● Albuminuria का इस्तेमाल diabetics में प्रारंभिक (incipient) nephropathy (the initial presence
of low but abnormal amounts of urine albumin) क
े detection क
े लिए एक चिह्नक (marker) क
े
रूप में करते हैं I
● यह cardiovascular disease क
े लिए एक स्वतंत्र चिह्नक (independent marker) क
े रूप में भी
इस्तेमाल होता है क्योंकि यह increased endothelial permeability का संक
े त देता है I
● यह chronic renal impairment का भी चिह्नक (marker) है I
Albuminuria test करने क
े लिए urine को सामान्यतः तीन तरीकों से collect किया जा सकता है :
● In a special container (with preservative) over a 24-hour period for urinary albumin
excretion (UAE) determination.
● A urine sample first thing in the morning or after a four-hour period of not urinating
(Timed urine test) for albumin excretion rate (AER) determination.](https://image.slidesharecdn.com/dmlt2kft-241225081037-2c451038/75/DMLT-2nd-Year-Kidney-Function-Tests-Some-basic-concepts-U-P-State-Medical-Faculty-syllabus-in-English-Hinglish-11-2048.jpg)
![14
Oxalate crystals - are present in ethylene glycol poisoning or primary and secondary
hyperoxaluria.
Cystine crystals - are observed in cystinuria
Glomerular Filtration Rate (GFR) - यह glomerular function का सबसे अच्छा सूचक (indicator) होता
है I GFR मिलिलीटर प्रति मिनट में वो दर (rate) होती है जिससे plasma क
े पदार्थ glomerulus क
े माध्यम से
filter होते हैं I एक व्यस्क (adult) में normal GFR 90 से 120 mL per minute होता है I
बहिर्जनित (Exogenous) markers of GFR -
● Inulin clearance - It involves the infusion of inulin (a small polysaccharide) and then the
measurement of blood levels of inulin after a specified period to determine the rate of
clearance of inulin. This is the 'reference method' for determining GFR.
● Other exogenous markers used are non-radioactive contrast agent, iohexol and
radioisotopes such as chromium-51 ethylene-diamine-tetra-acetic acid (51 Cr-EDTA),
and technetium-99m-labeled diethylene-triamine-pentaacetate (99 Tc-DTPA).
इन tests में अंतर्निहित असुविधा और इसक
े निष्पादन क
े लिए विशेष क
ें द्र की आवश्यकता क
े कारण GFR क
े
अंतर्जात (endogenous) markers क
े इस्तेमाल को अधिक प्रोत्साहन दिया जाता है I
अंतर्जात (Endogenous) markers of GFR -
Plasma/serum creatinine और urinary Creatinine - यह glomerular function क
े मूल्यांकन हेतु
आमतौर पर सबसे अधिक इस्तेमाल किया जाने वाला endogenous marker है I urinary creatinine क
े लिए
24 - घंटे में एकत्रित urine का इस्तेमाल करते हैं I चूंकि 24-घंटे की urine collect करना मुश्किल होता है और
इसमें गलती भी हो सकती है इसलिए बिल्क
ु ल सही - सही 5 से 8 घंटे में एकत्रित urine को प्राथमिकता दी जाती है
I Creatinine clearance is then calculated using the equation:
C = (U x V) / P
C = clearance, U = urinary creatinine concentration (mg/L) V = urinary flow rate (volume/time i.e.
ml/min), and P = plasma creatinine concentration (mg/L)
The creatinine clearance test is a method of assessing estimated GFR (eGFR).
[Important - Twenty-four-hour urine collection bottles may contain small amounts of
preservatives such as boric acid, hydrochloric acid, acetic acid, oxalic acid or thymol, and
therefore, the patient should be told that the direct contact with skin and mucous membranes
must be avoided]](https://image.slidesharecdn.com/dmlt2kft-241225081037-2c451038/75/DMLT-2nd-Year-Kidney-Function-Tests-Some-basic-concepts-U-P-State-Medical-Faculty-syllabus-in-English-Hinglish-14-2048.jpg)
![15
The creatinine clearance test का अब अधिक इस्तेमाल नहीं होता है, बल्कि इसक
े स्थान पर अधिकतर
eGFR equations का इस्तेमाल होता है जिनमें urine creatinine की जगह serum creatinine (SCr)
levels का प्रयोग करते हैं I
व्यस्को में, serum creatinine की मदद से glomerular filtration rate (GFR) estimate करने क
े लिए सबसे
व्यापक तौर पर इस्तेमाल होने वाली equations हैं - Chronic Kidney Disease Epidemiology
Collaboration (CKD-EPI) equation और isotope dilution mass spectrometry (IDMS) traceable
Modification of Diet in Renal Disease (MDRD) Study equation.
The CKD-EPI equation
GFR = 141 × min (Scr/κ, 1)α × max(Scr/κ, 1)-1.209 × 0.993Age × 1.018 [if female] × 1.159 [if
African American]
where:
Scr is serum creatinine in mg/dL,
κ is 0.7 for females and 0.9 for males,
α is -0.329 for females and -0.411 for males,
min indicates the minimum of Scr/κ or 1, and
max indicates the maximum of Scr/κ or 1
ये eGFR equations kidney function क
े मूल्यांकन हेतु अक
े ले serum creatinine levels से बेहतर होती हैं
क्योंकि इनमें race, age, and gender variables का भी समावेश होता है I eGFR equations are used to
determine the presence of renal disease, stage of CKD, and to monitor response to treatment.
—----------------------------------------------------------------------------------------------------------------------------
STAGES OF CHRONIC KIDNEY DISEASE GFR % OF KIDNEY FUNCTION
Stage 1 Kidney damage with normal kidney function 90 or high 90 - 100%
Stage 2 Kidney damage with mild loss of kidney function 89 - 60 89 - 60%
Stage 3a Mild to moderate loss of kidney function 59 - 45 59 - 60%
Stage 3b Moderate to severe loss of kidney function 44 - 30 44 - 30%
Stage 4 Severe loss of kidney function 29 - 15 29 - 15%
Stage 5 Kidney failure < 15 < 15%
—----------------------------------------------------------------------------------------------------------------------------
Serum creatinine - Creatinine, muscles में creatine phosphate का उप उत्पाद (by-product) है और
यह शरीर में एक constant rate से बनता रहता है I blood से अधिकांश creatinine kidneys द्वारा पूरी तरह से
साफ़ की जाती है I जब kidneys द्वारा creatinine की निकासी (clearance) कम होती है तो blood में
creatinine की मात्रा बढ़ जाती है और यह kidney function क
े ख़राब होने का एक संक
े त होता है I शरीर में प्रति
दिन उत्पादित creatinine की मात्रा शरीर क
े muscle mass और diet पर निर्भर करती है I हालांकि serum](https://image.slidesharecdn.com/dmlt2kft-241225081037-2c451038/75/DMLT-2nd-Year-Kidney-Function-Tests-Some-basic-concepts-U-P-State-Medical-Faculty-syllabus-in-English-Hinglish-15-2048.jpg)
![20
(xv) Serum creatinine का male व्यस्को में biological interval लगभग ____- ______ mg/dl और
female व्यस्को में लगभग ______ -_____ mg/dl होता है I
(xvi) Creatinine, muscles में creatine phosphate का ________ है I
(xvii) Urea protein metabolism और urea cycle क
े end product क
े रूप में _____ में बनता है I
(xviii) शरीर में urea का लगभग _____% kidneys द्वारा eliminate होता है और बाकी ___________ रास्ते
excrete होता है I
(xix) Urea का molecular weight ______ होता है I
(xx) BUN का full form _______________ है I
(xxi) Serum urea का स्तर BUN का लगभग _____ होता है I
(xxii) BUN का स्तर serum urea क
े स्तर का लगभग _______ होता है I
(xxiii) Serum urea मापने क
े लिए Chemical endpoint method का नाम है ________ method
(xxiv) Serum urea मापने क
े लिए Enzymatic endpoint method का नाम है ____________ method
(xxv) Serum Urea/BUN मापने का enzymatic kinetic method का नाम है ____________ method
(xxvi) UV GLDH method में GLDH का full form ____________ है I
(xxvii) व्यस्को में serum urea का reference interval _____ g/dl और BUN का reference interval
________ mg/dL होता है I
(xxviii) Cystatin C एक low-molecular-weight protein है जो शरीर की सभी ________ cells द्वारा
produce होती है I
(xxix) Creatinine की अपेक्षा ________ GFR का एक अधिक भरोसेमंद marker है क्योंकि यह age,
______ या diet से प्रभावित नहीं होता है I
(xxx) Serum Cystatin C का reference interval लगभग _______ mg/L होता है I
Ans. (i) albumin, (ii) pyuria, (iii) hematuria, (iv) hematuria, (v) alkaline, (vi) dehydration, (vii) 150,
(viii) 30, (ix) microalbuminuria, (x) microalbuminuria, (xi) muscle mass, diet, (xii) endogenous,
exogenous, (xiii) Jaffe's (xiv) 340, (xv) 0.9-1.3, 0.6-1.1 (xvi) by-product, (xvii) liver, (xviii) 85,
Gastrointestinal, (xix) 60, (xx) blood urea nitrogen, (xxi) दोगुना, (xxii) आधा, (xxiii) diacetyl
monoxime/DAM, (xxiv) Berthelot's, (xxv) UV GLDH, (xxvi) glutamate dehydrogenase, (xxvii)
15.6-46.8, 7-22, (xxviii) nucleated, (xxix) cystatin C, muscle mass, (xxx) 0.62 – 1.15
REFERENCES
1. Gounden V, Bhatt H, Jialal I. Renal Function Tests. [Updated 2023 Jul 17]. In: StatPearls
[Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK507821/
2. Gowda S et al. Markers of renal function tests. N Am J Med Sci. 2(4):170-173, 2010.
3. Nigam P K, Positive and negative false estimates of serum creatinine. Interventional
Cardiol 9(4):163-166, 2017.
4. Practical Clinical Biochemistry. Varley H, Gowenlock A H, Bell M. Fifth edition, 1991
5. Walmsley RN, Watkinson LR and Koay ESC. In: Cases in chemical pathology - a clinical
approach. Third edition World Scientific 1992.
Disclaimer : The pictures given in the text have been downloaded from Google images and I
am thankful to the persons who have uploaded these pictures.
Dr. P. K. Nigam
Ph. D. (Retired Biochemist)](https://image.slidesharecdn.com/dmlt2kft-241225081037-2c451038/75/DMLT-2nd-Year-Kidney-Function-Tests-Some-basic-concepts-U-P-State-Medical-Faculty-syllabus-in-English-Hinglish-20-2048.jpg)
