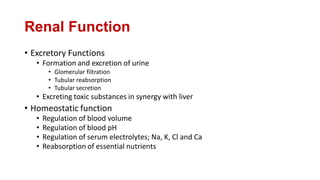
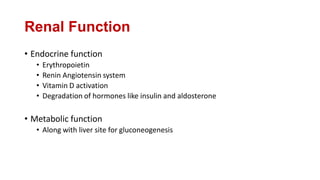
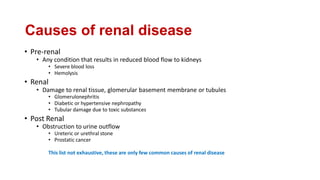
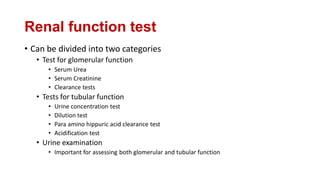
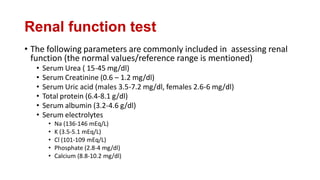
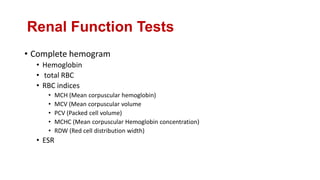
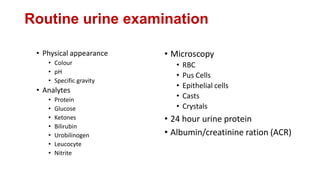
This document discusses renal function tests. It begins by listing the key functions of the kidney, including excretion, homeostasis, endocrine and metabolic roles. It then discusses various biochemical tests used to assess kidney function, including tests of glomerular function like serum creatinine and clearance tests, as well as tests of tubular function. Causes of renal disease including pre-renal, renal and post-renal are outlined. Normal ranges for common renal function biomarkers like serum urea, creatinine and electrolytes are provided. The document concludes by describing changes seen in results of hemogram, urine analysis and specialized clearance tests in the setting of kidney disease.
![Estimated GFR
• The Cockcroft-Gault formula for estimating creatinine clearance (CrCl)
is routinely as a simple means to provide a reliable approximation of
residual renal function in all patients with CKD. The formulas are as
follows:
• CrCl (male) = ([140-age] × weight in kg)/(serum creatinine × 72)
• However this has been extensively modified and there are online
calculators of eGFR from serum creatinine and body weight of
patients
• The eGFR is used to determine the stage of chronic kidney disease](https://image.slidesharecdn.com/renalfunctiontests-ppt-221005143547-0f925f3c/85/Renal-function-Tests-PPT-pdf-13-320.jpg)