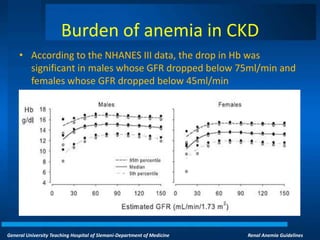
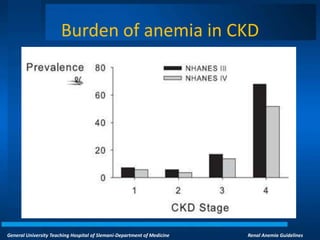
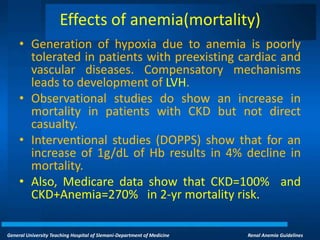
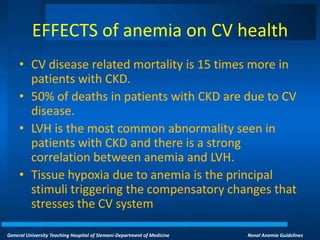
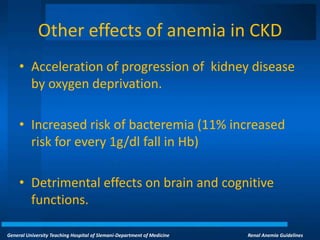
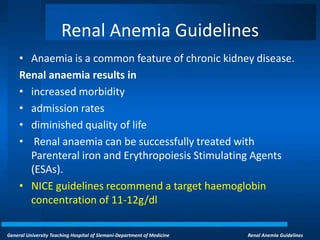
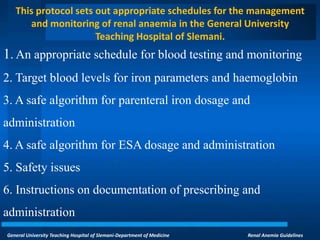
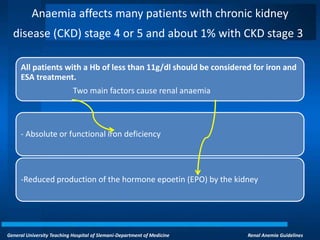
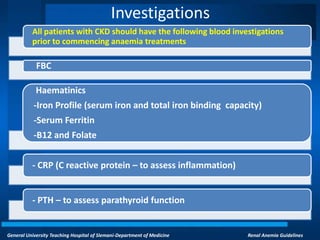
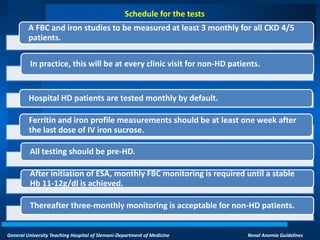
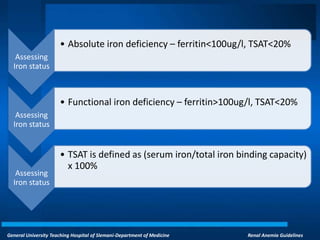
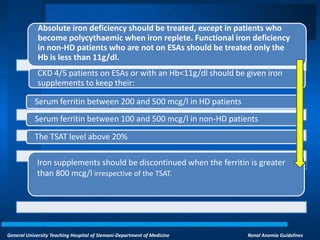
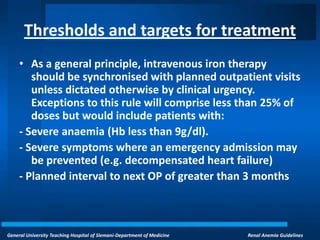
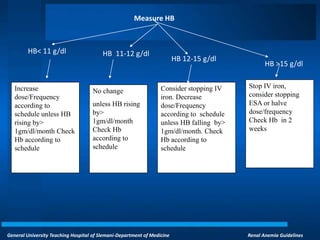
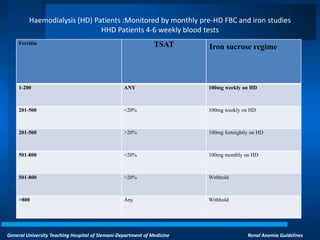
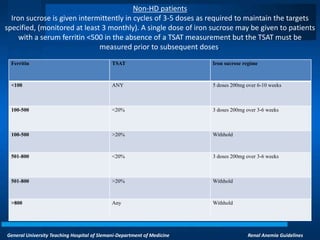
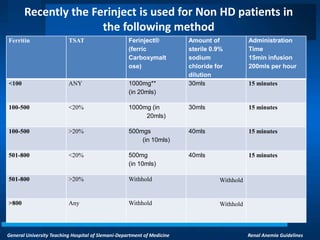
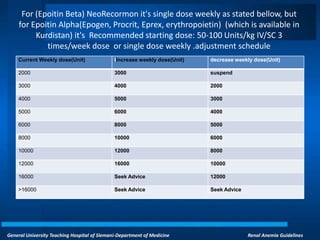
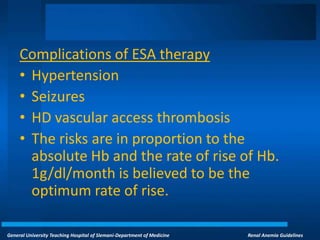
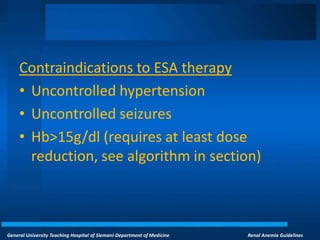
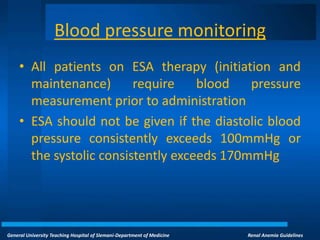
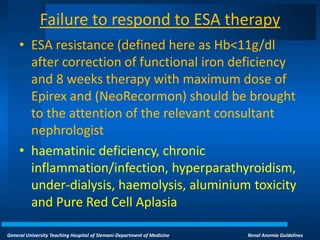
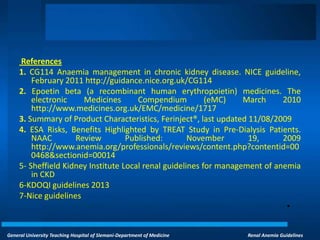
This document provides guidelines for managing anemia in chronic kidney disease patients at General University Teaching Hospital of Slemani. It outlines the historical background of understanding renal anemia and effects of anemia like increased mortality and cardiovascular disease. The guidelines recommend targets for hemoglobin concentration, iron status markers, and schedules for parenteral iron and erythropoiesis-stimulating agent administration and monitoring based on hemoglobin levels and dialysis status. Potential complications and contraindications of treatments are also discussed.