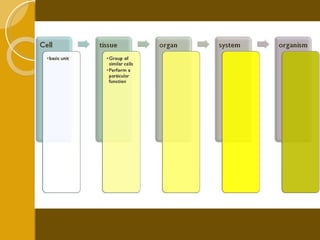
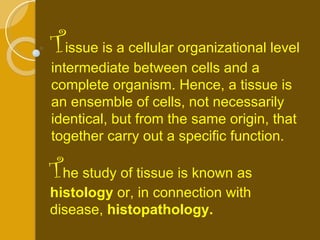
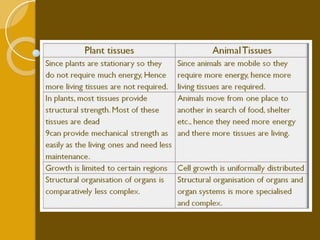
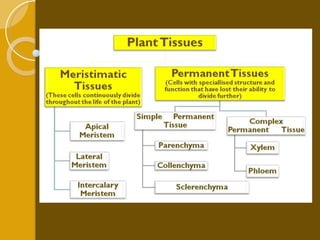
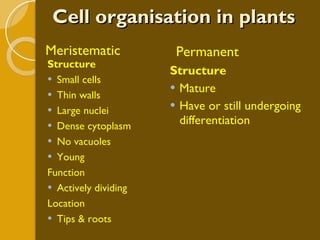
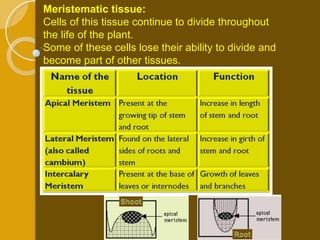
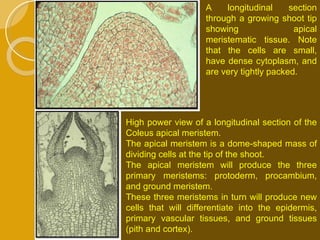
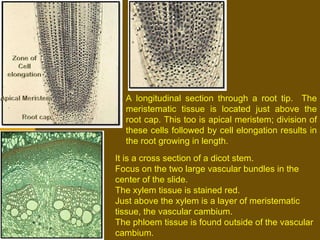
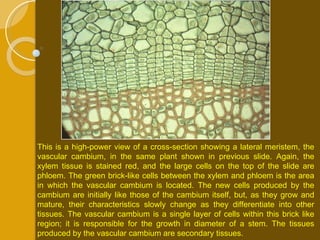
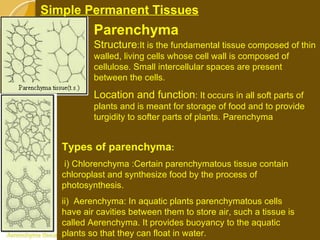
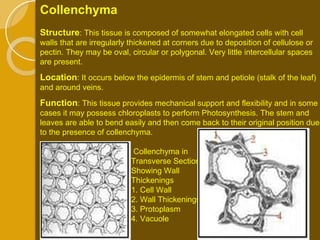
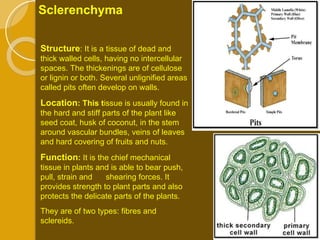
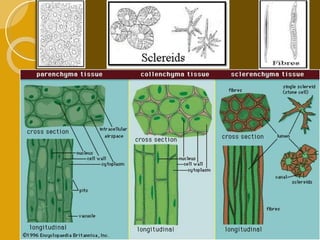
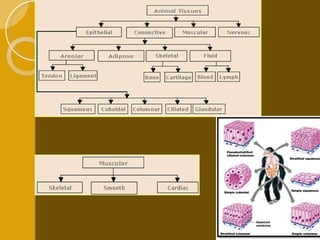
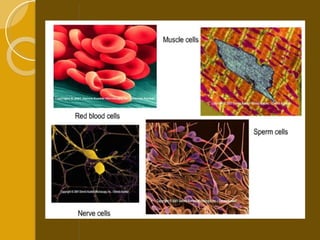
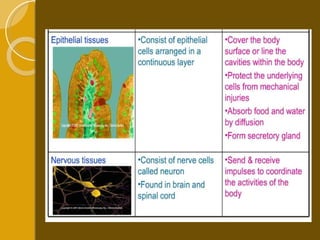
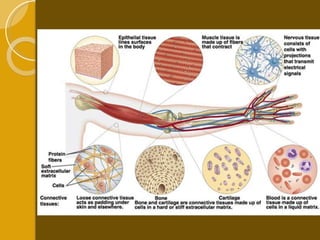
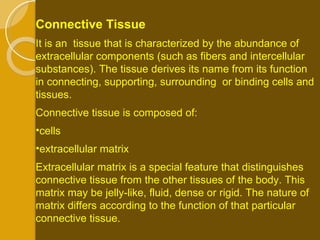
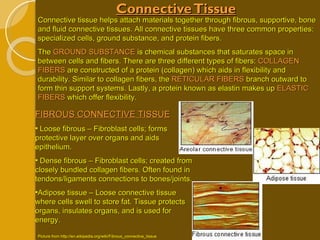
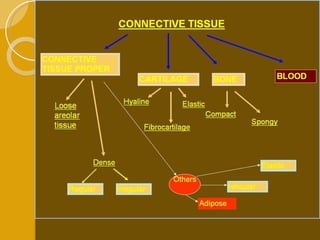
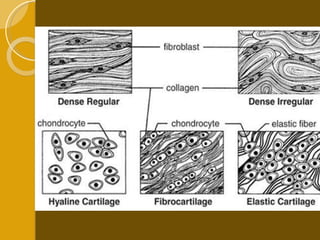
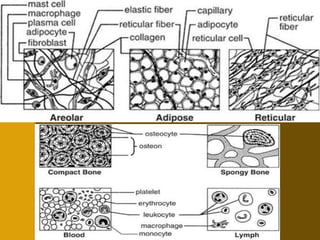
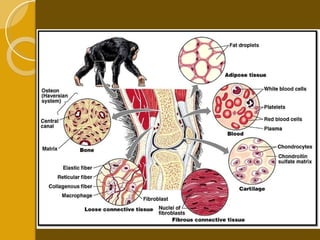
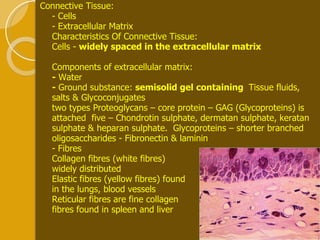
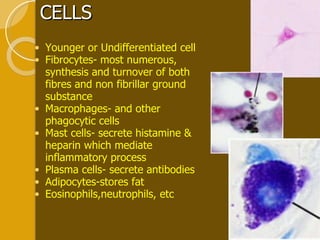
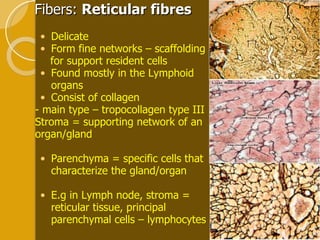
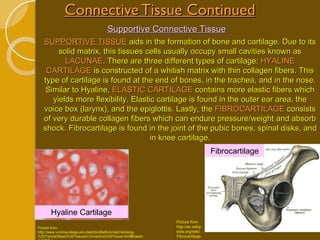
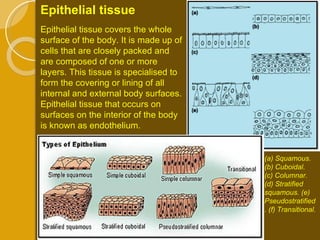
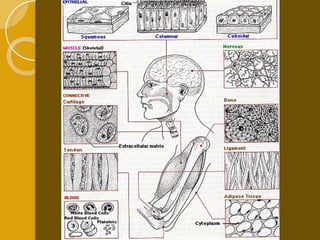
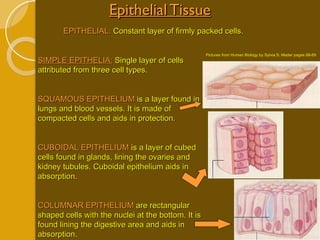
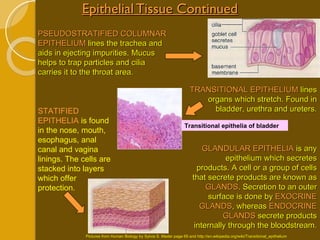
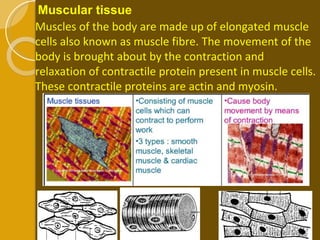
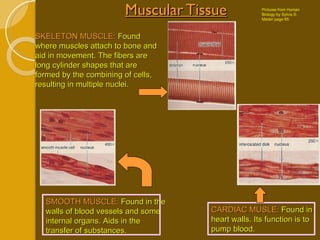
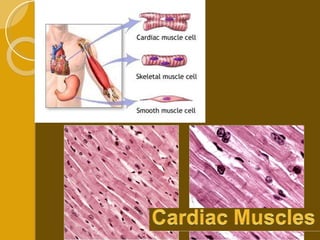
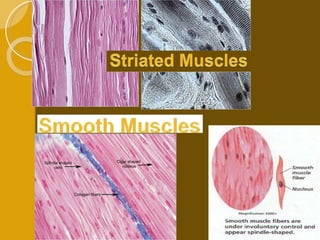
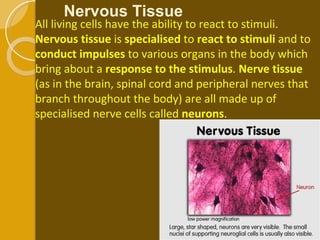
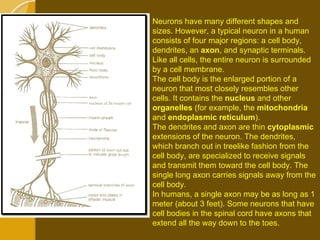
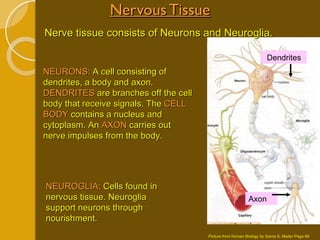
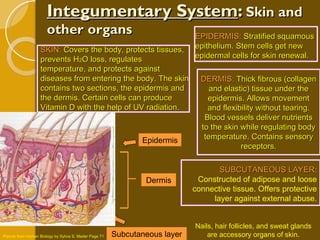
Cell specialization allows multicellular organisms to grow larger while dividing labor across specialized cell types and tissues. Tissues are groups of similar cells that work together to perform a common function. There are four main types of plant tissues - meristematic tissue which facilitates growth, permanent tissues including parenchyma for storage and transport, collenchyma for support and flexibility, and sclerenchyma for protection and strength. Animal tissues also specialize, with connective tissue binding other tissues, muscular tissue enabling movement, nervous tissue coordinating signals, and epithelial tissue covering and protecting organs.