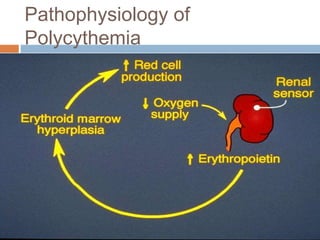
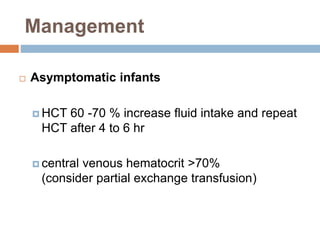
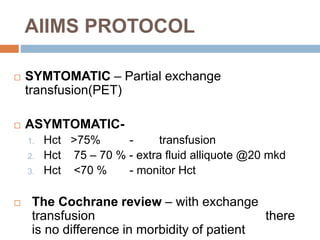
Polycythemia in newborns is defined as an increased total red blood cell mass with a hematocrit greater than 65%. This can lead to hyperviscosity or increased blood viscosity. Polycythemia occurs in 1-5% of term newborns, often due to placental transfusion or insufficiency. Clinical signs include poor feeding, lethargy, and hypotonia due to regional hypoxia from hyperviscosity or microthrombi formation. Asymptomatic infants with hematocrit 60-70% require increased fluids while those over 70% may need partial exchange transfusion. Symptomatic infants with hematocrit over 65% also receive partial exchange transfusion to reduce viscosity. The prognosis is