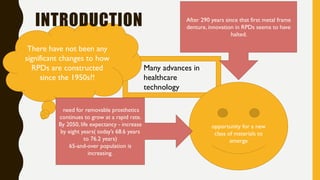
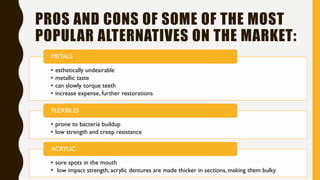
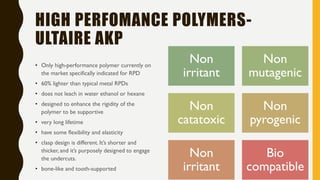
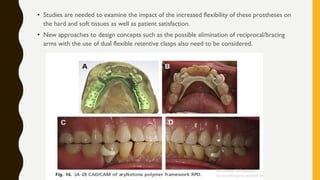
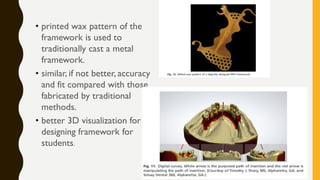
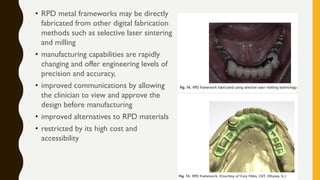
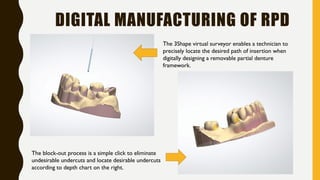
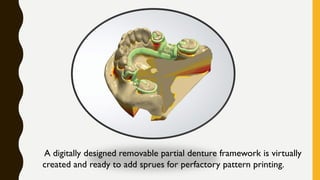
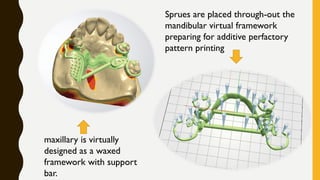
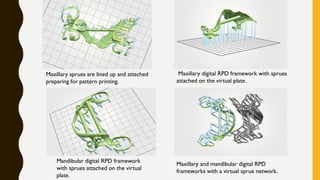
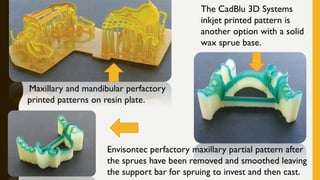
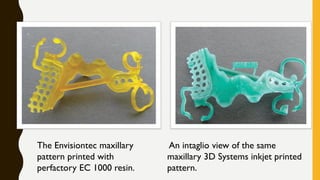
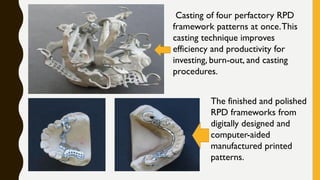
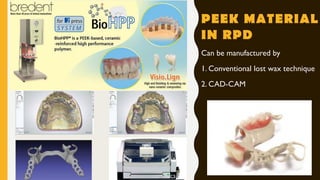
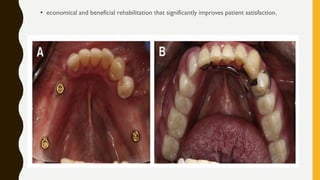
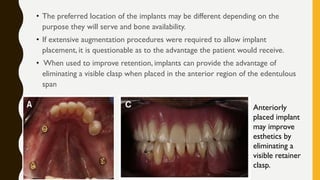
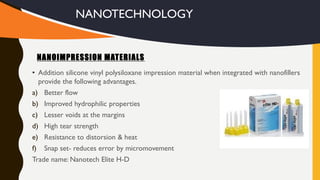
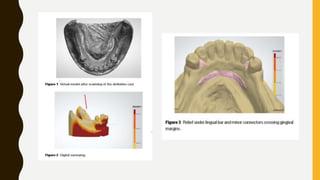
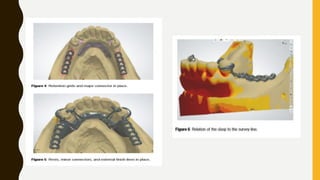
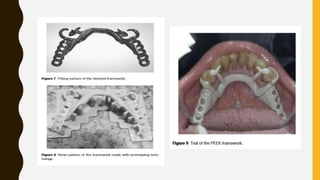
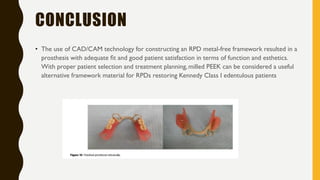
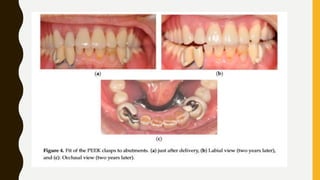
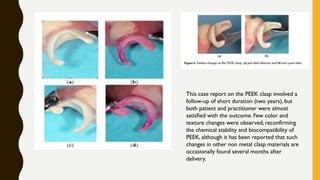
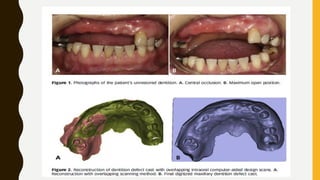
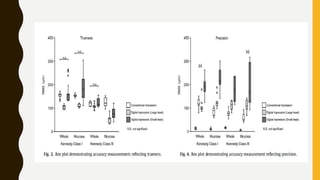
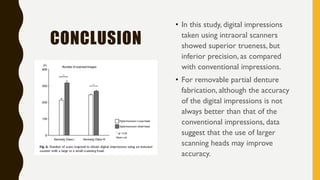
This document discusses recent advances in removable partial dentures (RPDs). It begins with an introduction noting that while healthcare technology has advanced, RPD design and fabrication has not significantly changed since the 1950s. It then discusses pros and cons of various materials commonly used for RPDs like metals, flexibles, and acrylic. New high performance polymers and CAD/CAM systems for digital design and manufacturing of RPD frameworks are also covered. The use of polymers like PEEK and implant-assisted RPDs to improve support, retention and stability is summarized. The document concludes with a review of the literature on the accuracy of CAD-CAM systems for RPD frameworks and a clinical case report on the use of 3D-printed