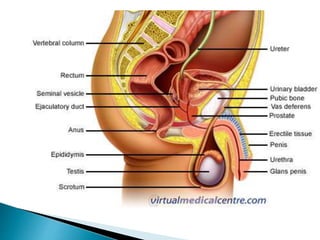
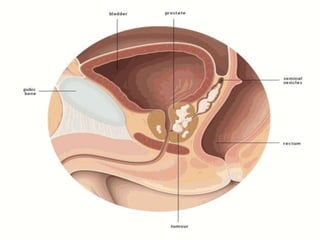
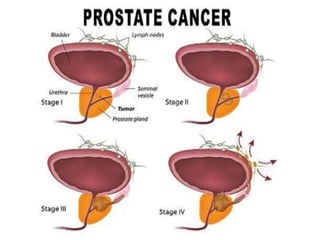
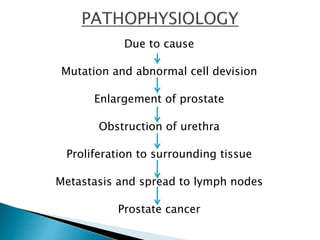
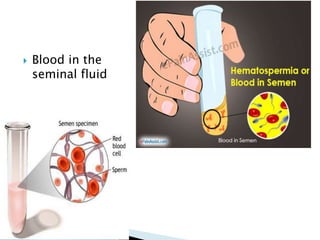
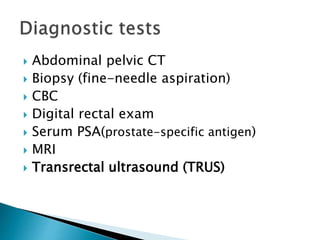
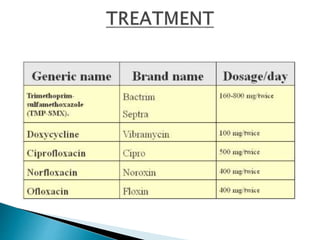
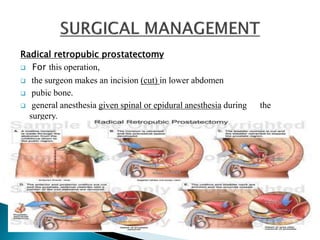
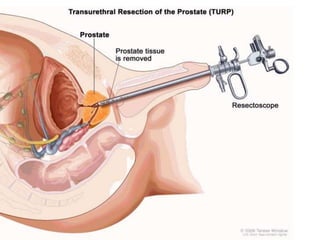
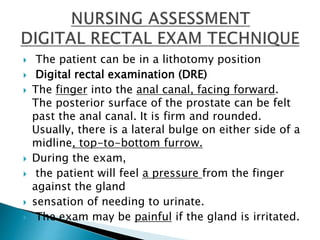
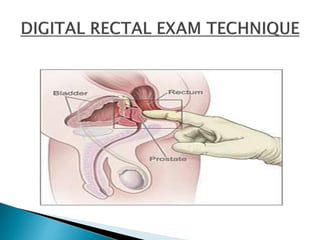
Prostate cancer is the uncontrolled multiplication of abnormal prostate gland cell tumor formation. It can be caused by genetic factors like family history or mutations, as well as increasing age and diet. Symptoms include frequent urination, blood in the urine or seminal fluid, and bone pain. Diagnostic tests include digital rectal exam, PSA testing, biopsy, and imaging. Treatment may include radical prostatectomy surgery or other options. Post-operative care focuses on urinary elimination, infection prevention, and nutrition management. Lifestyle changes like diet, exercise, and avoiding smoking can help prevention.