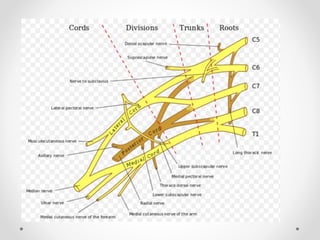
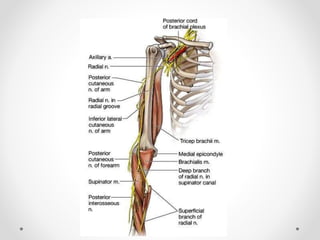
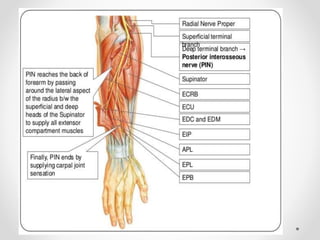
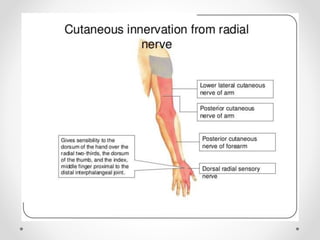
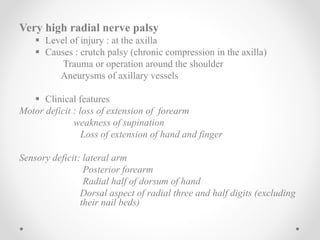
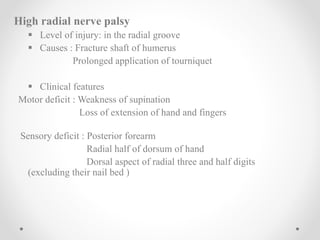
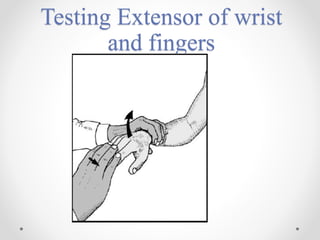
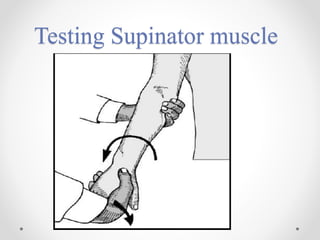
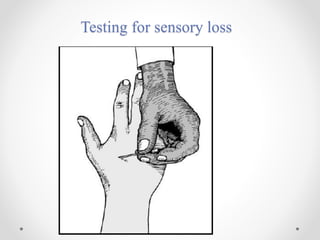
The radial nerve originates from the brachial plexus and provides motor and sensory innervation to parts of the arm and forearm. It has three main types of injury - very high (in the axilla), high (in the radial groove), and low (below the elbow). Clinical features depend on the level and include weakness of extension, supination, wrist drop and sensory loss over the back of the forearm and hand. Treatment involves nerve exploration, primary repair, delayed repair using grafts if needed, and tendon transfers if recovery is delayed. Prognosis depends on factors like age, nature of injury, level of lesion and surgical technique.