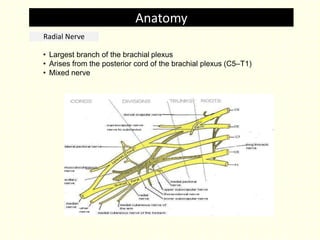
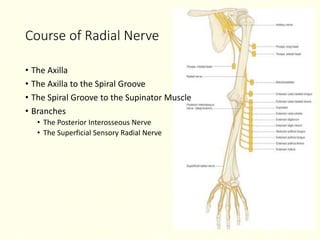
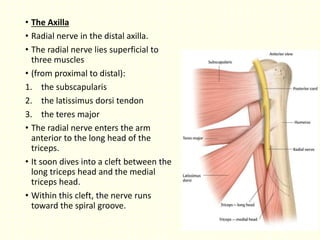
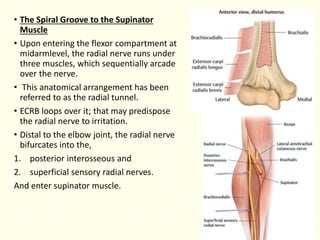
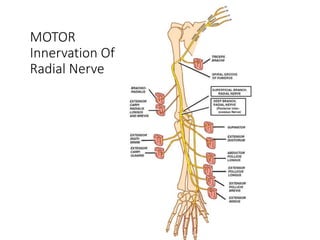
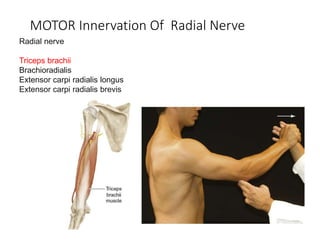
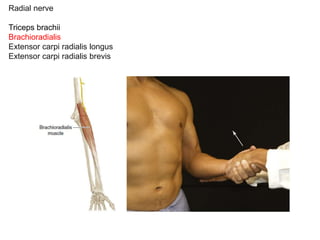
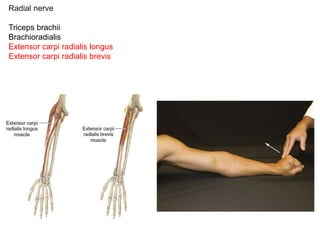
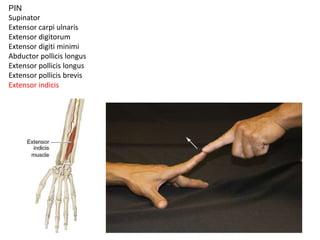
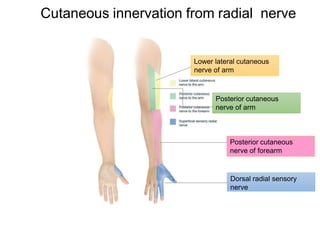
1. The radial nerve is a major branch of the brachial plexus that provides motor innervation to muscles of the posterior arm and extensor compartment of the forearm.
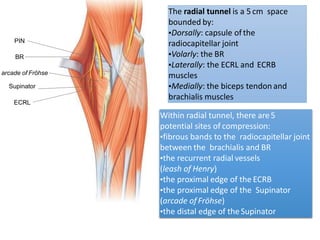
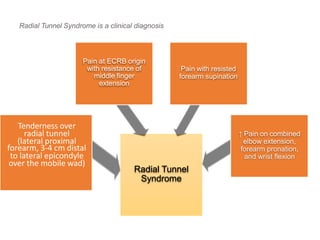
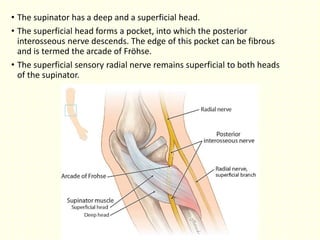
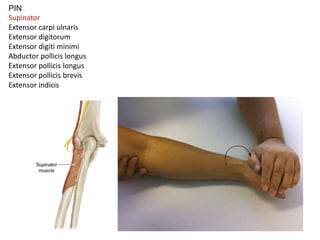
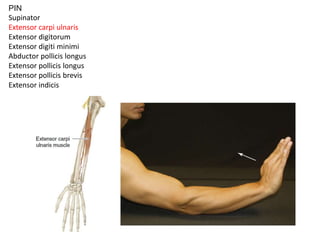
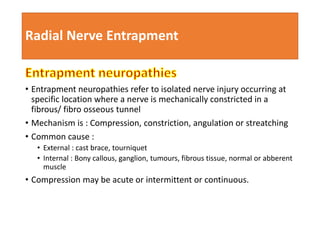
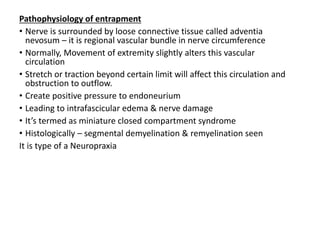
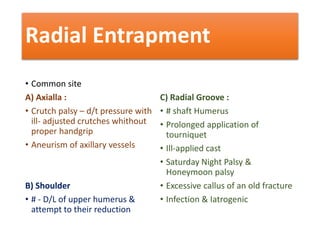
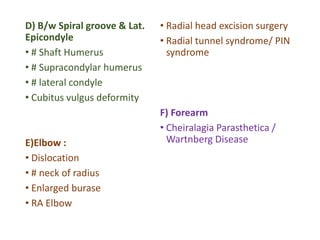
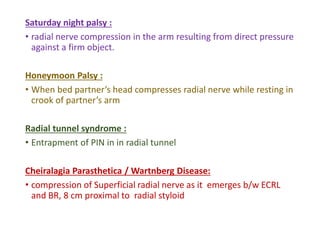
2. It is susceptible to entrapment at several points along its course, most commonly in the radial tunnel where the posterior interosseous nerve passes.
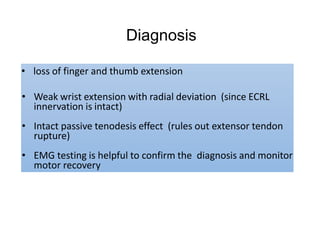
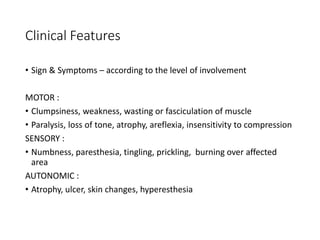
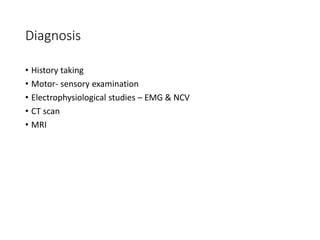
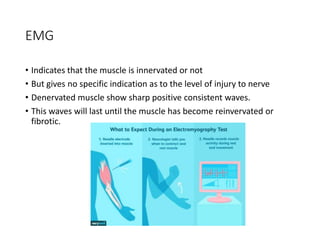
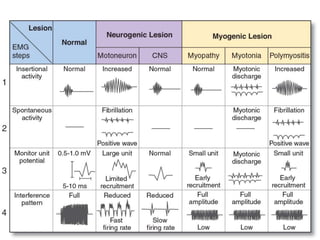
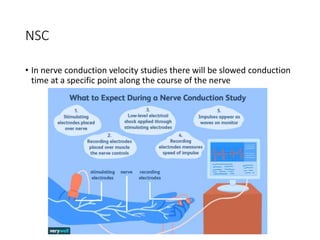
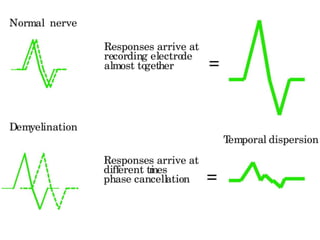
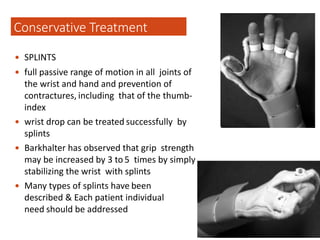
3. Radial nerve entrapment causes weakness of wrist and finger extension and can be diagnosed through history, physical exam including Tinel's sign, and electrodiagnostic testing. Conservative treatment includes splinting and steroid injections while surgery involves nerve decompression.
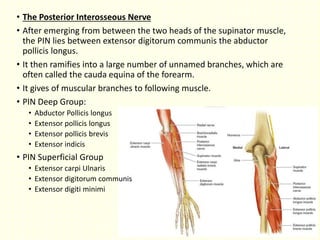
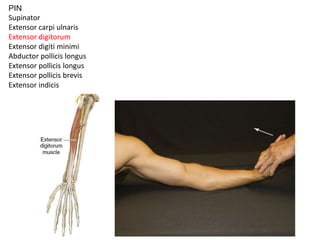
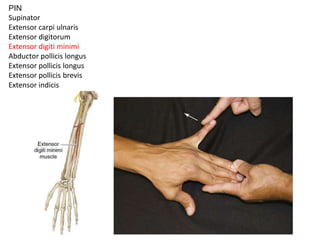
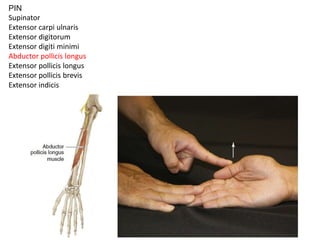
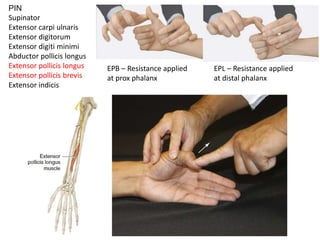
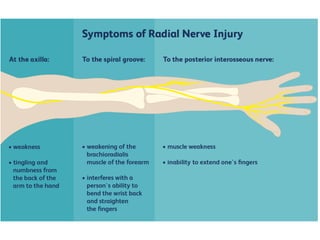

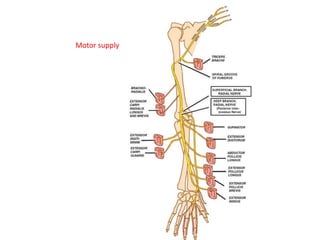
![ Tendon transplant in radial nerve palsy
needs to be provided with
(1) wrist extension.
(2) finger (metacarpophalangeal [MP] joint) extension.
(3) a combination of thumb extension and abduction.](https://image.slidesharecdn.com/radialnerveentrapment-200601154618/85/Radial-nerve-entrapment-48-320.jpg)