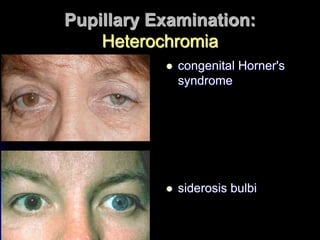
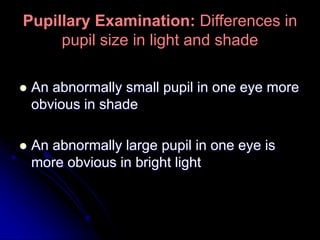
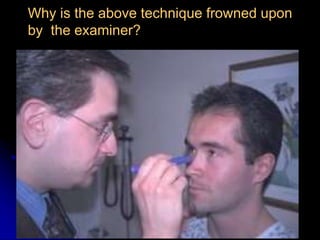
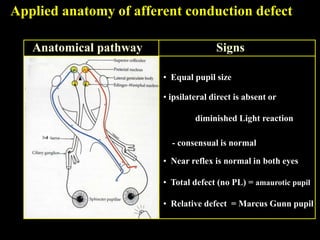
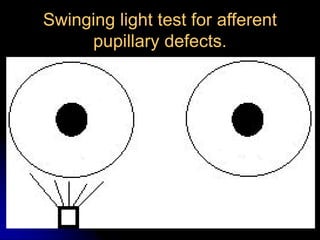
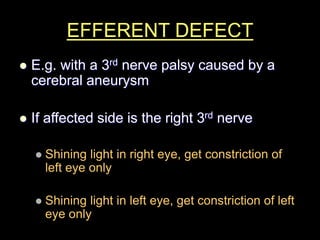
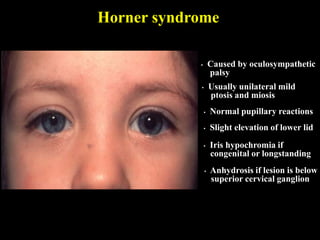
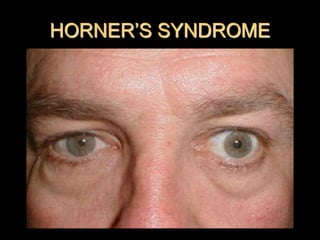
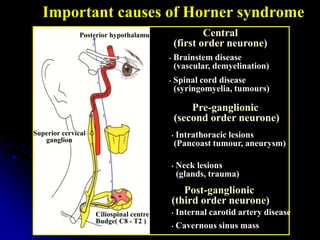
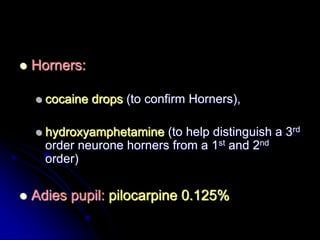
This document discusses examination of the pupils, including anisocoria, heterochromia, and pupillary reflexes. It describes evaluating pupil size in light versus dark, different neurological pathways, and potential causes of pupillary defects like Horner's syndrome. Specific tests are outlined, like the swinging light test for afferent defects and pharmacological tests to further evaluate pupil abnormalities.