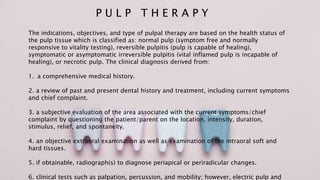
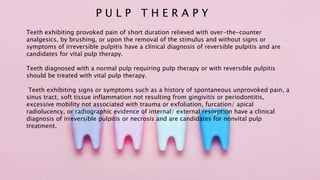
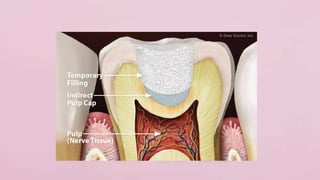
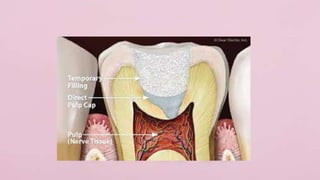
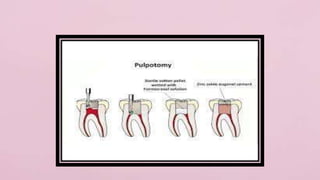
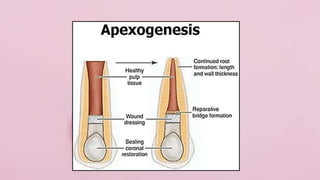
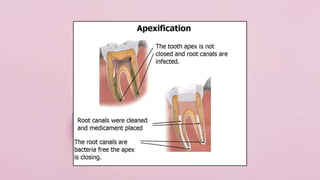
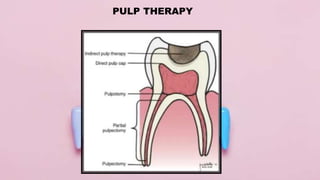
Pulp therapy aims to maintain tooth integrity and pulp vitality when possible. For primary teeth, this may involve indirect or direct pulp capping, pulpotomy, or pulpectomy depending on the pulp status and size of any exposure. For young permanent teeth, these same procedures plus apexogenesis or apexification may be used. Diagnosis is based on symptoms, history and testing to determine if the pulp is normal, reversibly inflamed, or irreversibly inflamed/necrotic to guide appropriate treatment. The goal is pulp or tooth preservation depending on prognosis.