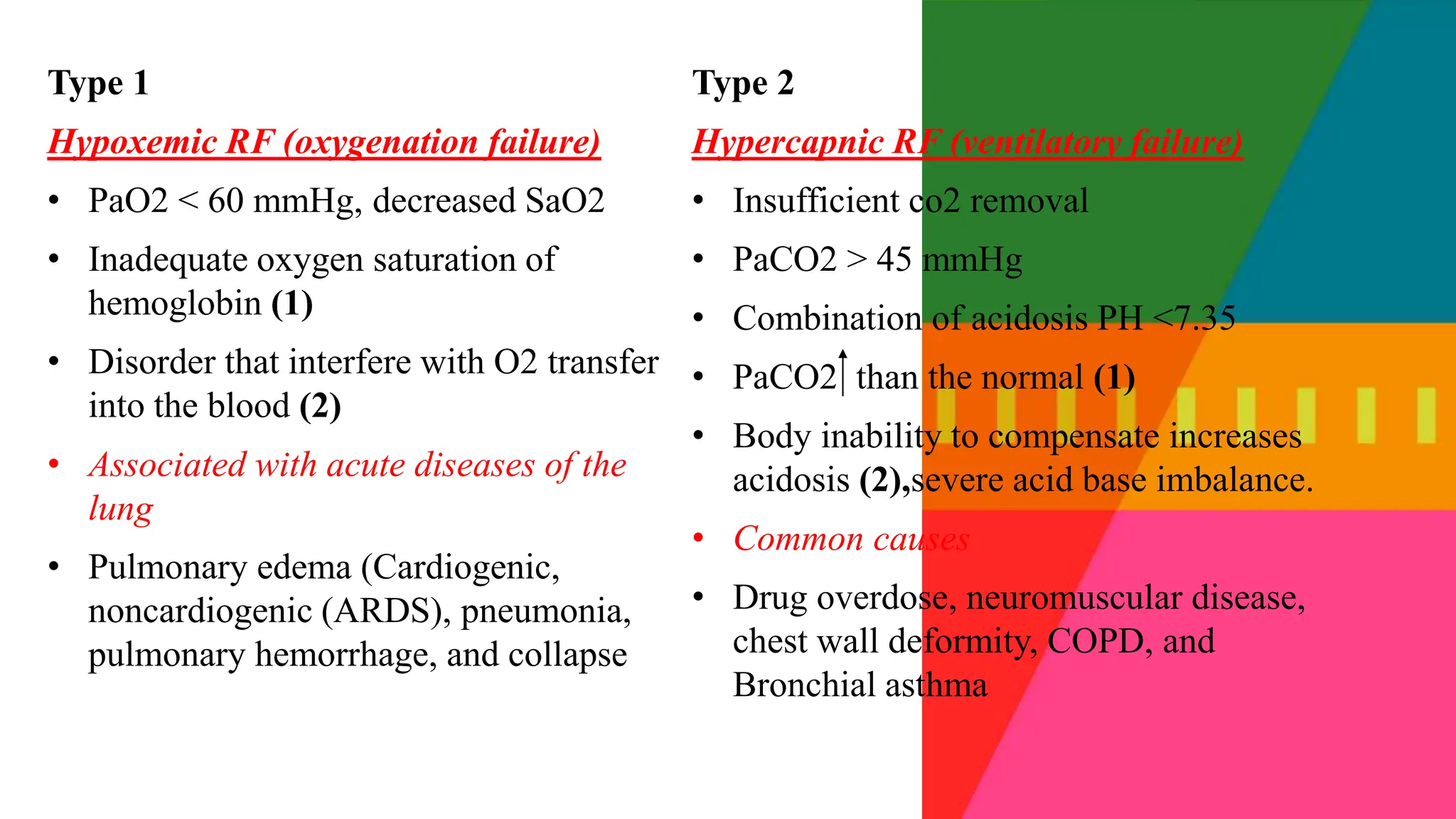
The document discusses acute respiratory failure and pulmonary embolism, highlighting the mechanisms, classifications, and causes of these conditions. It explains the differences between hypoxemic and hypercapnic respiratory failure, their pathophysiology, and the clinical manifestations associated with each. Additionally, it provides information on the diagnosis and management strategies for pulmonary embolism, including emergency interventions and long-term anticoagulant therapy.


































































![GENERAL MANAGEMENT- DRUG
THERAPY
Fibrinolytic agent
Unfractionated heparin IV
Low-molecular-weight heparin (e.g., enoxaparin [Lovenox])
Warfarin (Coumadin) for long-term therapy
Analgesia](https://image.slidesharecdn.com/acuterespiratoryfailure1autosaved-240613055024-837043a9/75/Acute_respiratory_failure-1-Autosaved-pptx-68-2048.jpg)








