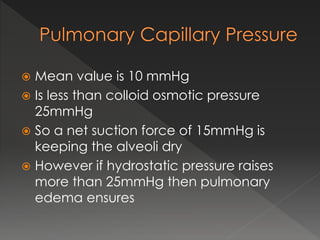
The pulmonary circulation has several key characteristics:
1) It has low pressure and resistance but high compliance, allowing the lungs to accommodate large blood volumes.
2) Pulmonary blood flow increases with elevated pulmonary arterial pressure due to recruitment of new vessels and increased vessel distension.
3) Hydrostatic pressures in the lungs vary based on posture, creating three zones of blood flow.