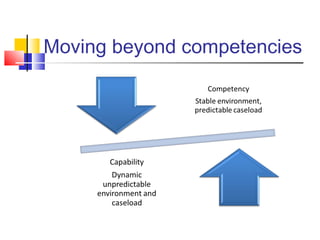
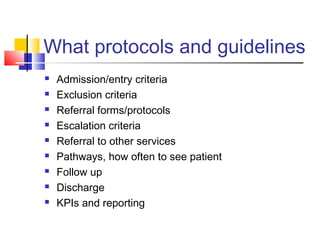
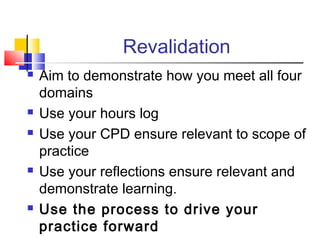
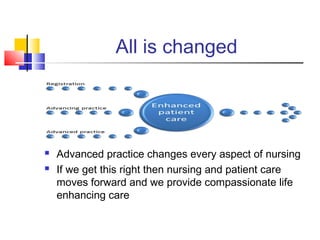
This document discusses competency development and revalidation for advanced nursing practice. It aims to help those managing advanced practice nurses understand the components of advanced practice and how to support nurses' skills development. It defines advanced practice nursing and outlines the core competencies including autonomous practice, clinical decision making, and prescribing. It provides guidance on maintaining and enhancing skills through education, mentoring, and experience. It also addresses setting up nurse-led services, developing guidelines, and preparing for revalidation through appraisal and continuing professional development.