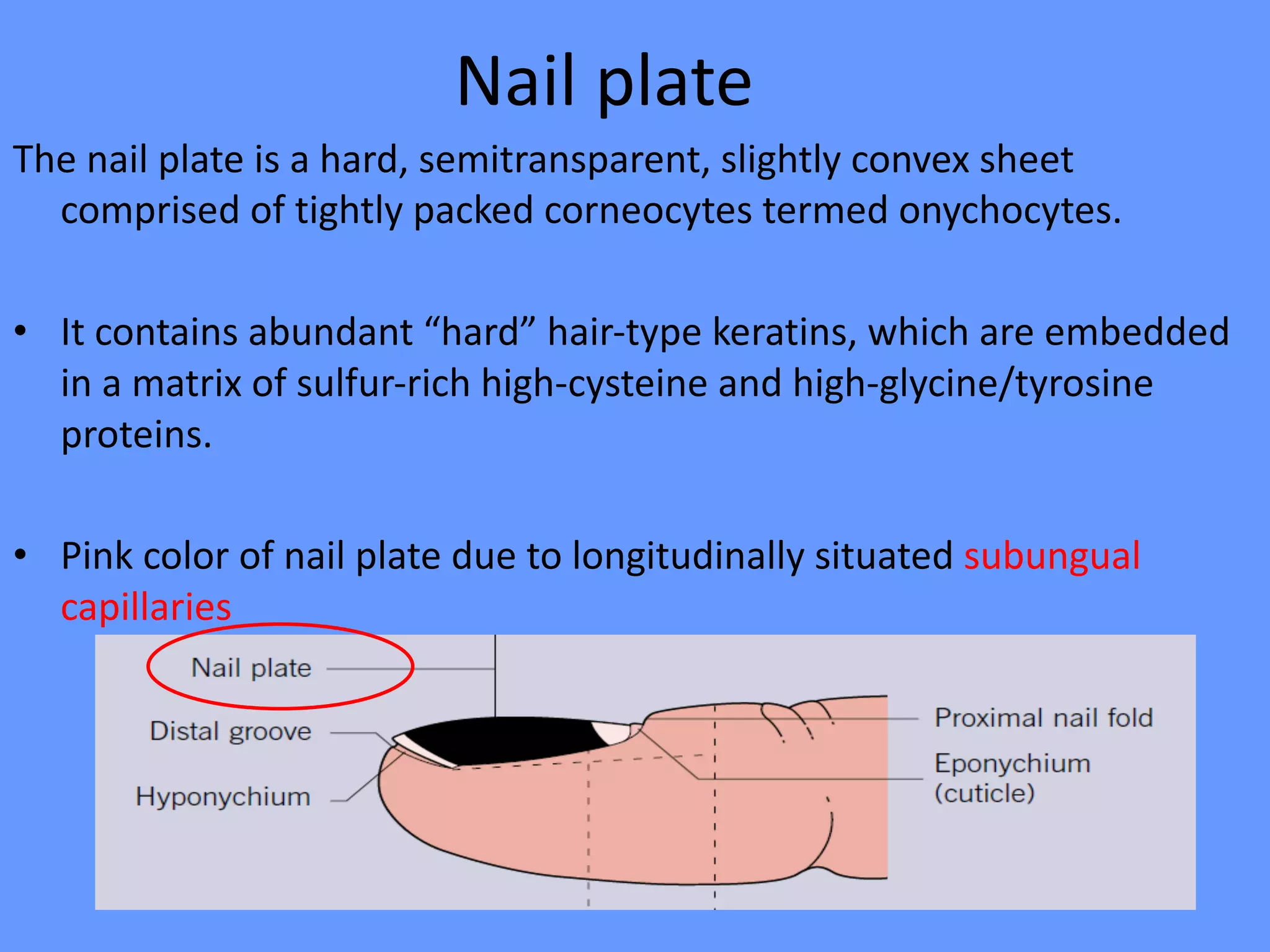
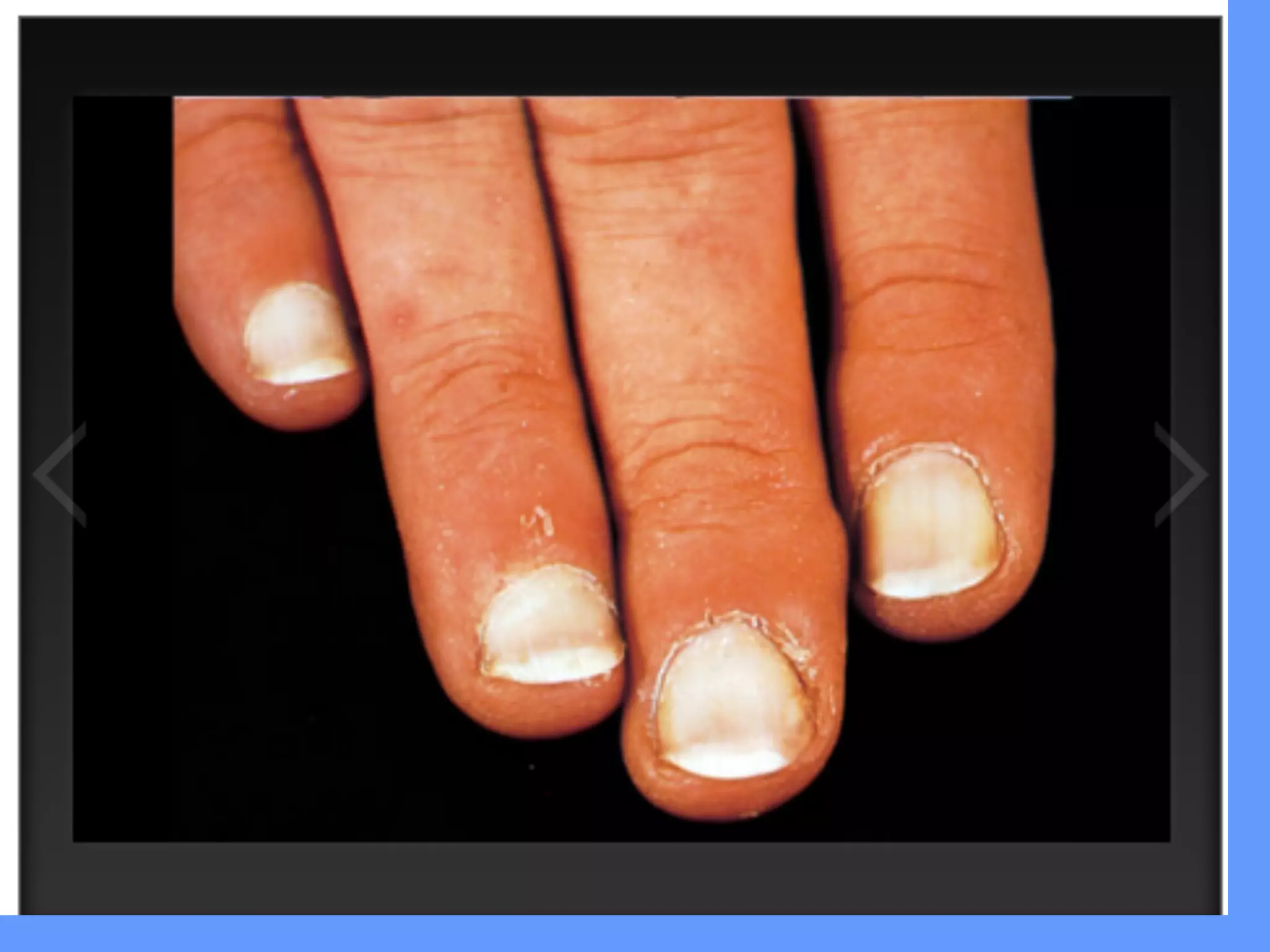
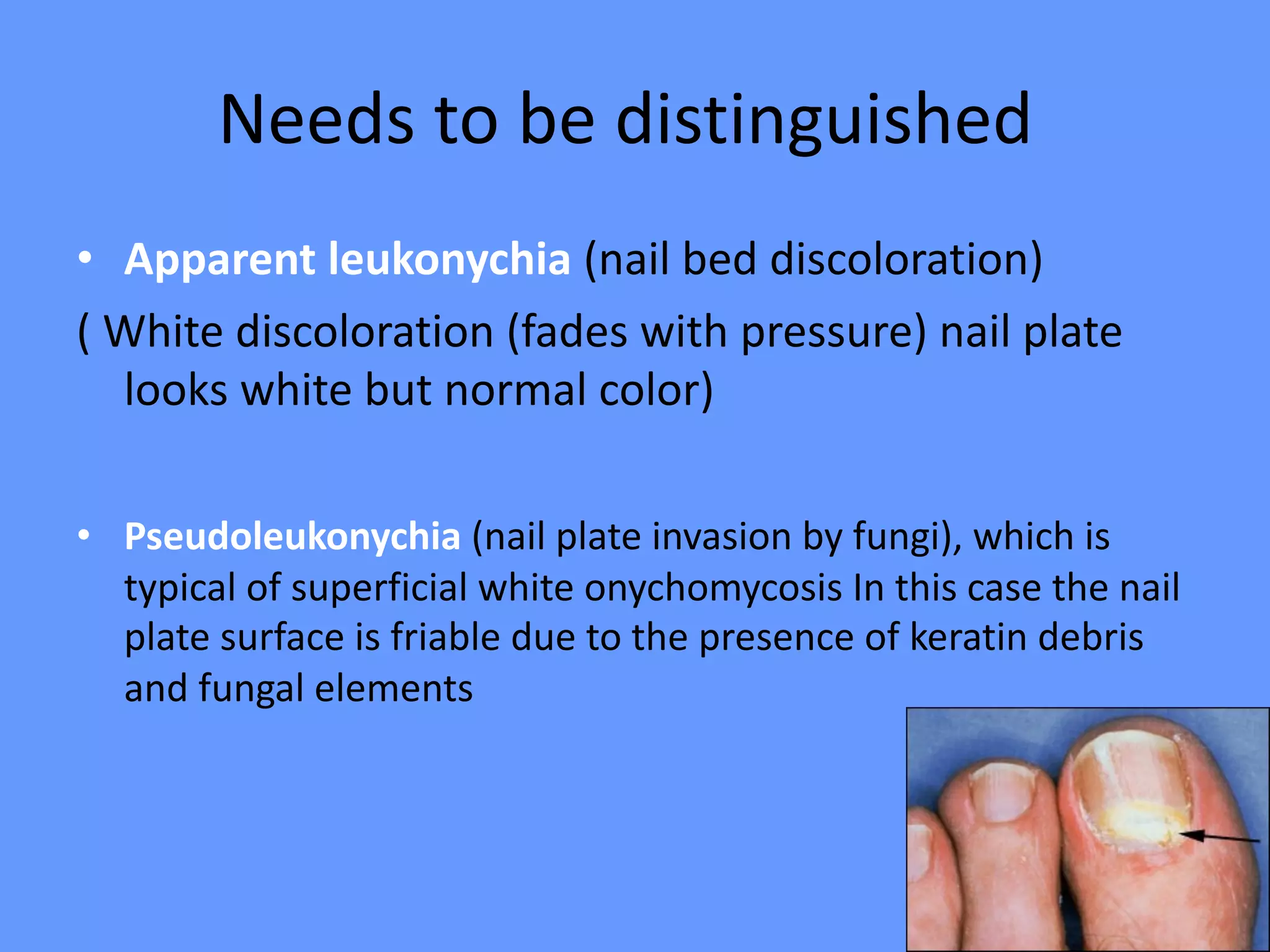
This document discusses nail anatomy and disorders. It begins by describing the anatomy of the nail unit including the nail plate, nail bed, cuticle, matrix, and lunula. It then discusses various nail disorders and abnormalities such as Beau's lines, leukonychia, pitting, and onychomycosis. For each abnormality, it provides the description, potential causes, and associated area of the nail apparatus. Common infections like paronychia and pseudomonas are also summarized. The document concludes with a brief discussion of nail tumors.