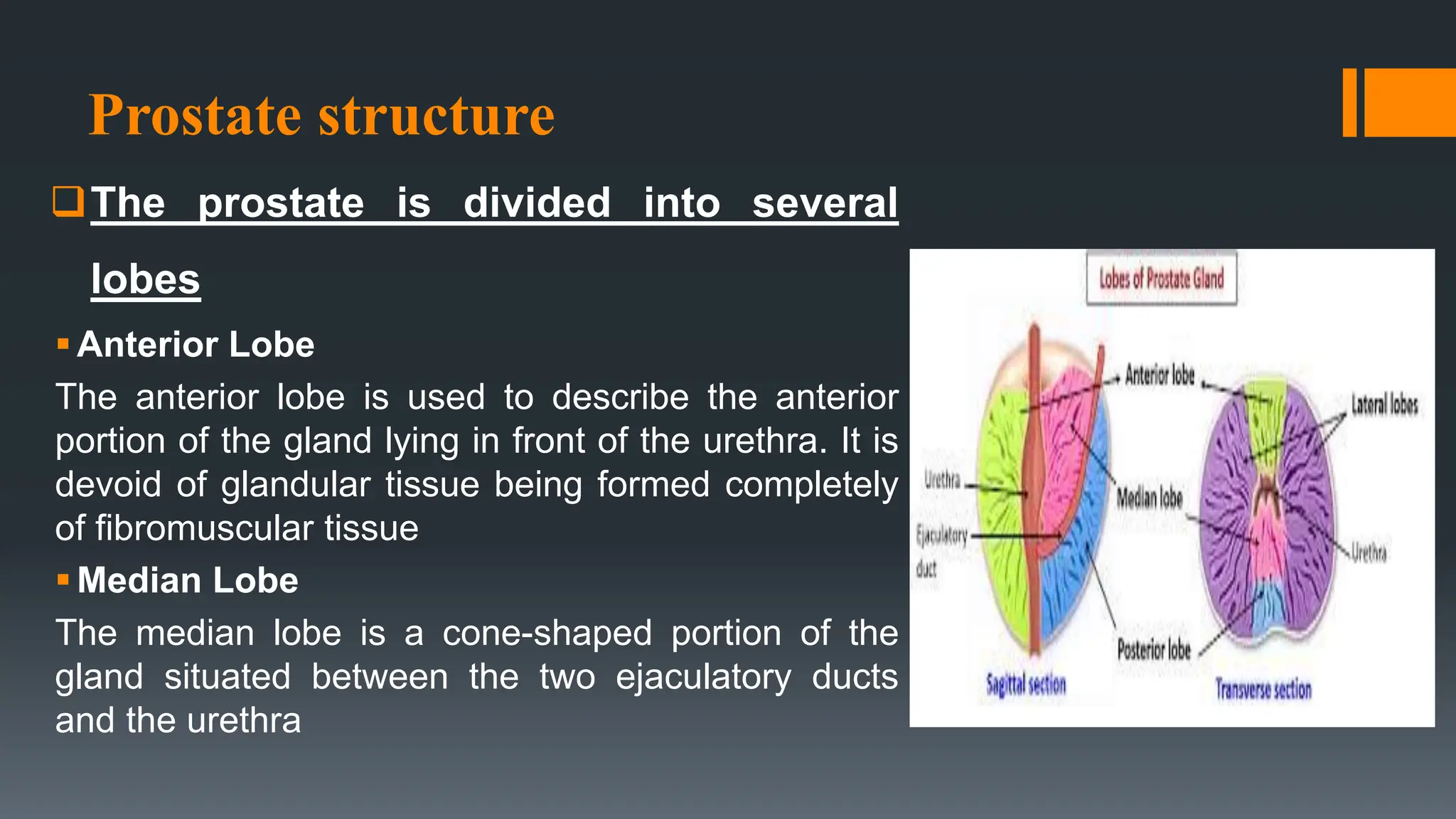
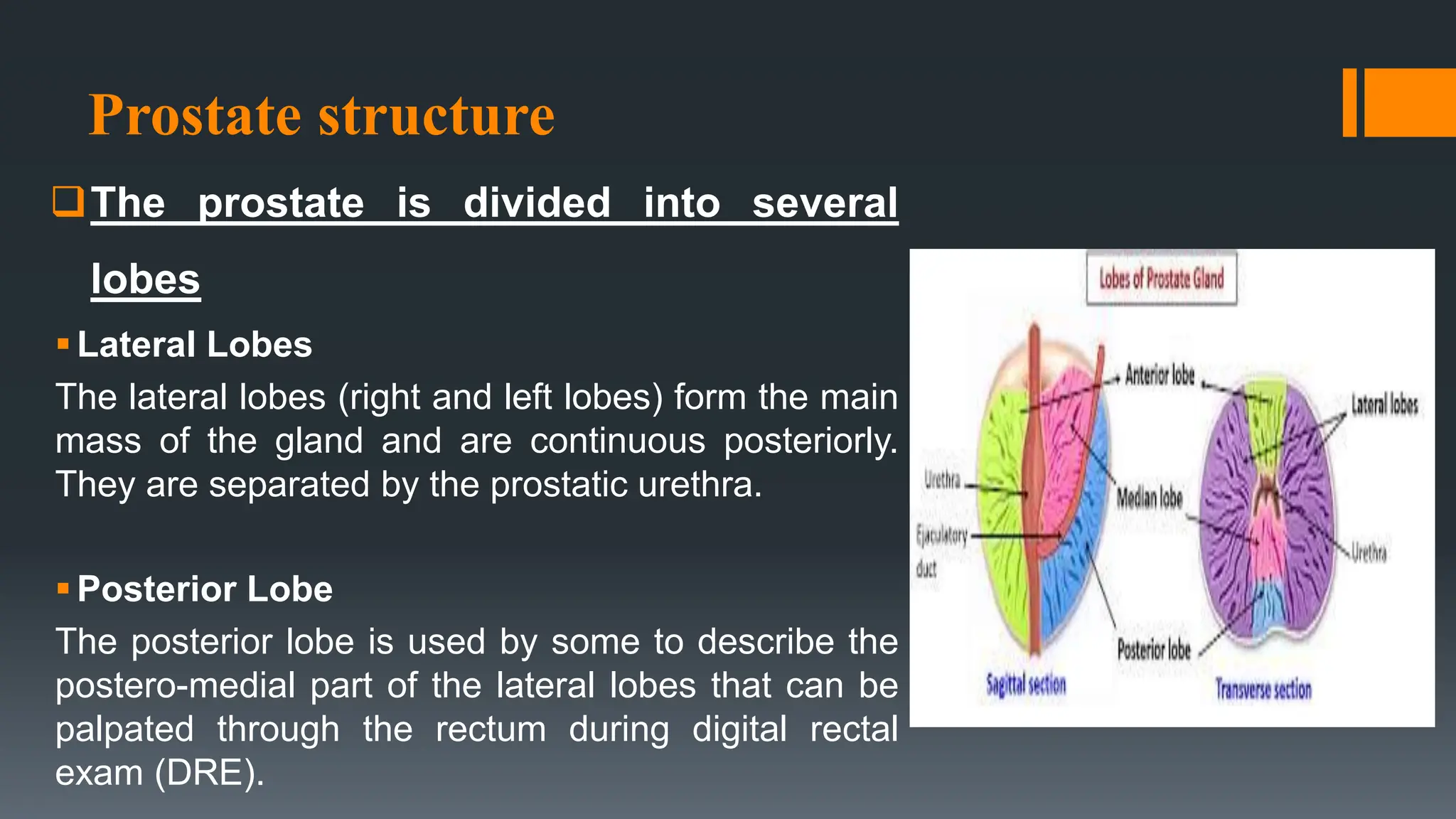
The document provides an extensive overview of the prostate, including its anatomy, physiology, common conditions such as benign prostatic hyperplasia (BPH) and prostatitis, and prostate cancer. It discusses the prostate's structure, its role in semen production and urinary control, various diagnostic tests, surgical procedures like prostatectomy, and potential complications. Additionally, it outlines various forms of urinary incontinence and physical therapy interventions to manage these conditions.