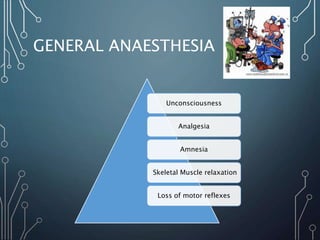
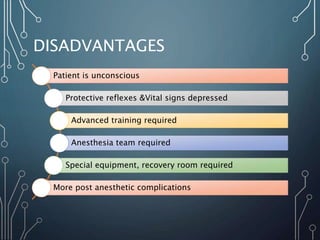
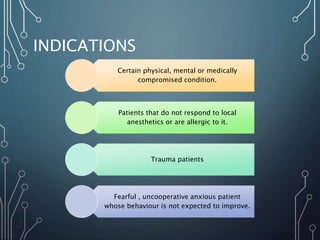
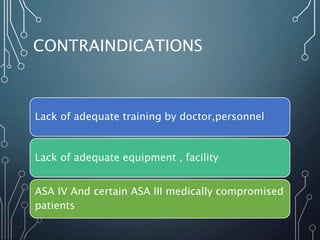
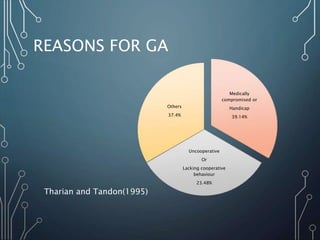
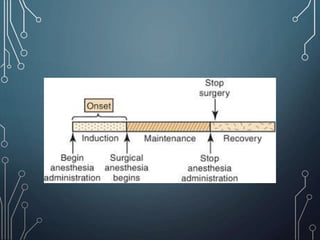
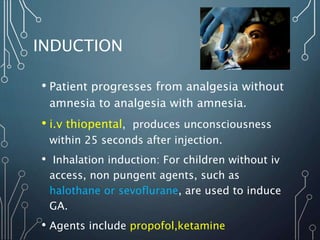
General anesthesia involves inducing a state of unconsciousness through administration of anesthetic agents to provide analgesia, amnesia and muscle relaxation for surgical procedures. It allows treatment of uncooperative patients or those with medical conditions making local anesthesia unsuitable. Proper pre-operative evaluation, monitoring during induction and maintenance of anesthesia, and post-operative care are essential for safe administration of general anesthesia.